You don’t want to be figuring things out while your chest is tight and every breath feels like a small battle. A written plan turns panic into steps. You’ll know what to take, when to take it, when to check peak flow, and when to call for help. It won’t prevent every flare, but it will cut the chaos and shorten attacks. That’s the goal here: a simple plan you can follow under pressure.
TL;DR - Your Fast-Track Plan
Keep this short list on your phone’s lock screen or in your wallet.
- Know your green/yellow/red zones: green (>80% of personal-best peak flow, or no symptoms), yellow (50-79% or symptoms), red (<50% or severe symptoms).
- At the first sign of bronchospasm: use your rescue inhaler (albuterol/levalbuterol) 2-4 puffs with a spacer. Repeat every 20 minutes for up to 3 rounds in the first hour if needed. If you were prescribed an ICS-formoterol inhaler for both relief and control, follow your clinician’s “as-needed” use and daily maximum.
- Recheck symptoms/peak flow 10-20 minutes after treatment. If you’re not clearly improving, escalate per your plan (add controller, consider oral steroid if your clinician has given you a “rescue steroid” plan, or head to urgent care/ER).
- Call emergency services now if you’re struggling to speak in full sentences, lips/fingernails look blue, chest feels “silent,” you’re drowsy/confused, or your peak flow stays <50% after rescue medicine.
- Put your plan in writing, stock a go-kit (inhalers + spacer + peak-flow meter), train a buddy/family member, and set refill reminders.
Build Your Personal Plan (Step-by-Step)
This section turns the big idea into actions you can print and follow. It’s built around the typical “zones” approach used in asthma care because bronchospasm is often part of asthma, exercise-induced bronchoconstriction, or COPD flares.
First, a quick note: This is educational. Your plan should be signed off by your clinician. Medication names and ranges below reference standard guidance from GINA (Global Initiative for Asthma 2024-2025), NHLBI (2020 Focused Updates), and GOLD (for COPD, 2025). Always use the exact inhalers and doses your clinician prescribes.
1) Nail down your baseline and triggers.
- Get your “personal best” peak flow. Measure twice daily for 2-3 weeks while you feel well. The highest reliable number becomes your personal best.
- List triggers that tighten your airways: viral colds, pollen, dust, smoke, pets, cold air, exercise, perfumes/cleaners, reflux, or stress. Note what specifically sets you off. Be concrete (e.g., “cut grass,” “winter running,” “cat dander”).
- Know your pattern. Are your attacks fast and sharp (minutes) or slow burn (hours to days)? Do nights or early mornings hit harder? Patterns guide prevention.
2) Choose your medicines with your clinician.
- Rescue: short-acting beta-agonist (SABA) like albuterol or levalbuterol. Make sure you have a spacer and know how to use it.
- Controller: inhaled corticosteroid (ICS), sometimes paired with formoterol (an ICS-LABA combo). Many people use ICS-formoterol both daily and “as-needed” (SMART/MART strategy) per GINA.
- Add-ons when needed: long-acting muscarinic antagonist (LAMA), leukotriene modifiers, or biologics for allergic/eosinophilic asthma (clinician decision).
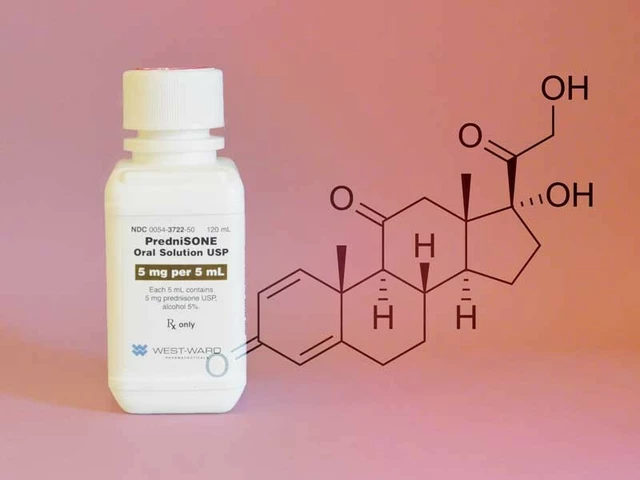
- Rescue steroid plan (if appropriate): a short course of oral steroids (e.g., prednisone/prednisolone). This should be pre-specified with clear start criteria and dose written on your plan.
- Nebulizer: useful if you struggle with inhaler technique or during bad flares. Keep the tubing, masks, and power source ready.
3) Write your zone-based actions.
- Green Zone (steady): take your daily controller exactly as prescribed. Warm up before exercise. If you have exercise-induced bronchospasm, your plan might include 2 puffs of albuterol 5-15 minutes before activity or an ICS-formoterol puff before activity (if prescribed that way).
- Yellow Zone (worsening): cough, chest tightness, wheeze, or peak flow 50-79% of personal best.
- Red Zone (danger): very short of breath, trouble speaking, ribs pulling in, “silent chest,” or peak flow <50%.
4) Fill in your exact steps for each zone.
- Yellow Zone typical steps (confirm with your clinician):
- Take rescue inhaler 2-4 puffs with a spacer. Shake, seal lips, press once, slow deep breath, hold 10 seconds, wait 30-60 seconds between puffs. Recheck in 10-20 minutes.
- If your plan uses ICS-formoterol “as-needed,” take the number of puffs your clinician wrote. Do not exceed your personal daily max on the label/plan.
- Add your “yellow step-up” controller intensification if your clinician has included it (often extra ICS doses for a few days).
- Hydrate, avoid triggers (step away from smoke, cold air), and consider a warm room and pursed-lip breathing.
- If not clearly improving after 1 hour or you need rescue again within 3 hours, escalate (clinic/urgent care or the red zone protocol).
- Red Zone typical steps:
- Take rescue medication now. If using a SABA: 4-8 puffs with spacer, or nebulized albuterol if you have it and were told to use it. If you use ICS-formoterol for relief, follow the red-zone number on your plan.
- Start your oral steroid “rescue pack” if your clinician has prescribed one and told you when to start it. Common adult examples: prednisone 40-50 mg once daily for 5 days; child dosing is weight-based and must be written by the clinician (often 1-2 mg/kg/day, max typically 40 mg). Do not self-start without prior instructions.
- If you’re not better in 15-20 minutes, or you’re getting worse at any point, call emergency services. Do not drive yourself if you’re very short of breath.
5) Make it real-life proof.
- Carry it: one rescue inhaler lives on you; one lives at home; one lives at work/school. Check expiry dates every month.
- Spacer: always use one for metered-dose inhalers. It increases lung delivery and shortens attacks.
- Peak-flow meter: keep it in your go-kit. Log readings in your phone. The trend matters.
- School/work: give a copy of your plan to the nurse/HR. For kids, ask about a school asthma/allergy action plan and self-carry permission if appropriate.
- Allergy season or cold/flu waves: pre-stock medications before peak season. Keep masks on hand for cold air or viral spikes.
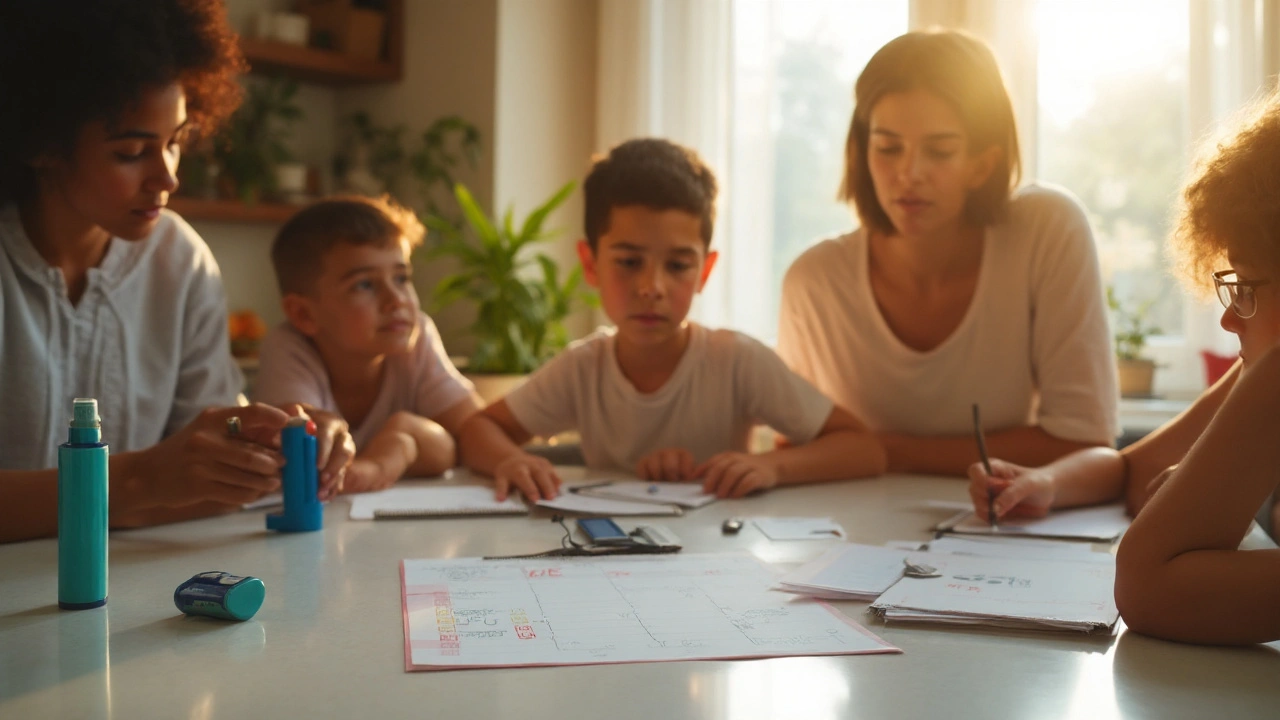
6) Train your circle and schedule reviews.
- Teach one person your plan. Quick drill: you describe symptoms; they fetch inhaler/spacer; they count your puffs and start a timer; they know when to call 911.
- Review the plan after any ER visit, oral steroid course, or big life change (new job, new city, pregnancy). Plans age. Refresh them.

Examples, Checklists, and Cheat Sheets
Use these examples to shape your one-page plan. Edit them to match your exact prescriptions.
Example adult plan (as a template you’d customize):
- My personal-best peak flow: 520 L/min (green ≥416; yellow 260-415; red <260).
- Rescue inhaler: albuterol 90 mcg MDI + spacer. Yellow: 2-4 puffs; may repeat in 20 minutes (up to 3 rounds first hour). Red: 4-8 puffs now; call for help if not better in 15-20 minutes.
- Controller: budesonide-formoterol 160/4.5: 2 puffs morning and night. As-needed relief: 1 puff for symptoms as instructed, not exceeding my written daily max.
- Oral steroid: Prednisone 50 mg daily x 5 days (start if red zone or per clinician note). Start only if I hit the start criteria written on my plan.
- Triggers to avoid: cigarette smoke, outdoor runs in cold dry air, dusting without a mask, colds (hand hygiene, flu/COVID shots on schedule).
- Emergency markers: can’t speak a full sentence, ribs pulling in, blue lips, faint/drowsy, peak flow <260 after treatment. Call emergency services.
Example child plan (template; needs pediatric dosing from clinician):
- Personal best: 250 L/min (green ≥200; yellow 125-199; red <125).
- Rescue: albuterol MDI with spacer and mask. Yellow: 2 puffs; repeat every 20 minutes up to 3 rounds in the first hour as needed. Red: 4-8 puffs now; call for help if not better in 15 minutes.
- Controller: daily ICS or ICS-formoterol as prescribed; as-needed relief per the written pediatric plan (max daily puffs specified by clinician).
- Rescue steroid: prednisolone at child’s weight-based dose if the clinician wrote start criteria; begin only per plan.
- School: plan on file with nurse; inhaler/spacer available; parent/guardian contacts updated.
Quick inhaler technique (MDI + spacer):
- Shake the inhaler. Attach to spacer. Exhale away from the spacer.
- Seal lips around spacer mouthpiece (or use mask snugly for kids).
- Press the inhaler once; breathe in slowly and deeply; hold 10 seconds.
- Wait 30-60 seconds before the next puff. Rinse mouth after ICS use.
Dry powder inhaler (DPI) pointers:
- Exhale away from the device before loading the dose.
- Seal lips; inhale fast and deep. No spacer for DPIs.
- Hold 10 seconds; close and store dry. Rinse if it contains steroid.
Red flags that override the plan (call emergency services now):
- Blue/gray lips or nails; severe breathlessness; can’t speak in full sentences.
- Peak flow <50% personal best that doesn’t bounce back after rescue meds.
- Rescue inhaler not lasting at least 3 hours between doses during a flare.
- Drowsiness, confusion, or a “silent chest” (very quiet breathing).
- History of ICU/intubation for asthma or sudden bad flares.
Common triggers and how to blunt them:
- Colds/viruses: hand hygiene, sleep, masks in crowded indoor spaces during spikes, current flu and COVID vaccines per age/eligibility.
- Allergens: dust-mite covers, wash bedding hot weekly, HEPA filter, keep pets out of the bedroom, close windows during high pollen, shower after outdoor exposure.
- Smoke/air quality: avoid smoke; check AQI; use a respirator mask (e.g., during wildfire days); run air purifier.
- Exercise: longer warm-up, pre-exercise inhaler as prescribed, scarf over mouth/nose in cold air.
- Reflux: smaller meals, avoid late-night eating, raise head of bed, ask about reflux treatment if symptoms are frequent.
- Medications: ask your clinician about non-selective beta-blockers or NSAIDs if they’ve triggered symptoms in you.
Cheat sheet: your zone table (print this). Values below are typical; replace with your own numbers and prescriptions.
| Zone | Peak Flow | Symptoms | Actions | Medicines (examples; use your exact plan) |
|---|---|---|---|---|
| Green | >= 80% of personal best | No cough/wheeze/tightness; sleeping fine; normal activity | Keep doing what works; warm-up for exercise; avoid triggers | Daily controller as prescribed; pre-exercise puff if on plan |
| Yellow | 50-79% | Cough, mild wheeze, chest tightness, waking at night | Use rescue now; recheck in 10-20 minutes; consider step-up; monitor closely | SABA 2-4 puffs with spacer, may repeat q20 min up to 3 rounds in 1 hour; or ICS-formoterol as instructed for relief; short step-up of ICS if on plan |
| Red | <50% | Very short of breath, ribs pulling in, trouble speaking, blue lips, “silent chest” | Rescue now; start emergency steps; call emergency services if not improving in 15-20 minutes or worsening | SABA 4-8 puffs with spacer or nebulizer per plan; ICS-formoterol per red-zone instructions; start oral steroid if clinician provided a rescue pack; oxygen in medical setting |
One-page checklist to tape inside a cabinet:
- My personal-best peak flow: ____ L/min; Green ≥ ____; Yellow ____-____; Red < ____.
- My rescue inhaler is: ____; my spacer is in: ____; both replaced/checked on the 1st of each month.
- My daily controller is: ____; dose: ____; time: morning ____ / night ____.
- As-needed plan: ____; maximum daily puffs: ____ (from clinician).
- Rescue steroid: ____ mg for ____ days; start if: ____; call clinic when started.
- Emergency triggers for 911: blue lips, can’t speak full sentences, peak flow red after treatment, drowsy/faint.
- Contacts: clinician ____; emergency contact ____.
Mini‑FAQ and Troubleshooting
What if I don’t have my inhaler with me? A few things help in a pinch: stop and rest, breathe through pursed lips (in through nose for 2-3 seconds, out through pursed lips for 4-6 seconds), sip room‑temp water, get to warmer humid air if cold air set you off, and remove yourself from triggers (smoke, perfume). Caffeinated drinks can mildly help some people, but this is not a substitute for medication. Get access to your inhaler or urgent care fast.
Should I use a nebulizer or a metered-dose inhaler? With a spacer and correct technique, an inhaler delivers medicine just as well as a nebulizer for most people. Nebulizers are helpful if you’re too tight to coordinate breaths, for young kids, or during heavy flares. Use what you and your clinician prefer for your plan.
What’s the difference between albuterol rescue and ICS-formoterol “SMART” use? Albuterol opens airways fast. ICS-formoterol combines quick-opening with steroid to calm inflammation. Many adults and teens now use ICS-formoterol as both their daily controller and their reliever. Your plan should state which approach you’re on and list the maximum daily puffs.
Can anxiety trigger bronchospasm? Yes. Fast breathing and panic tighten airways and chest muscles. Use a brief grounding routine (sit, elbows on knees, slow nose-in/pursed-lips-out breathing, eyes on a fixed point). Then follow your plan. If anxiety is a recurring trigger, add a coping strategy to your written plan and ask your clinician about options.
Is steam helpful? Warm humid air can feel soothing, especially if cold dry air triggered you, but steam doesn’t replace medication and is risky for small children (burns). Focus on your plan first.
What about COPD and smoking-related bronchospasm? The zone approach still helps, but medications and targets differ. If you have COPD, build your plan with your clinician using GOLD 2025 guidance. Smoking cessation, vaccines, and pulmonary rehab are high-impact steps.
Do I need vaccines? Respiratory viruses are common triggers. Staying current with flu and COVID vaccines (per local guidelines and your clinician’s advice) lowers the odds of severe flares.
Any meds I should ask about? If you’ve had issues with NSAIDs (like aspirin) or non-selective beta-blockers in the past, bring that up. Your clinician can tailor options.
Pregnancy? Many inhaled controllers and rescue medicines are used safely during pregnancy, but your obstetric and lung/asthma teams should co-manage your plan. Don’t stop medicines without talking to them.
Travel tips? Pack double: one rescue inhaler in your pocket, one in your bag. Bring spacer, peak-flow meter, copies/photos of your plan, and a letter listing your meds. On planes, keep meds in carry-on. Check air quality and pollen at your destination.
How often should I update the plan? At least yearly, and after any emergency visit or steroid course. If you’re using rescue more than twice a week (outside of pre-exercise use), ask for a controller review.
Quick decision tree when symptoms hit:
- Symptoms? Stop activity. Sit upright. Check if you have your inhaler/spacer.
- Take rescue per plan. Start a timer for 10-20 minutes.
- Reassess: better and staying better? Move back to green steps and avoid triggers.
- Not better or getting worse? Repeat rescue (if allowed), step up per plan, and prepare to call or go in.
- Any emergency sign at any time? Call emergency services now.
Sources that shape these steps: Global Initiative for Asthma (GINA) 2024-2025 strategy reports; U.S. NHLBI 2020 Focused Updates to Asthma Management Guidelines; Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2025 reports; and guidance from the American Academy of Allergy, Asthma & Immunology. Your local clinician’s advice always comes first.
Last thing: write it down. A plan you can point to beats a plan you “sort of remember.” Take five minutes today, fill in the blanks with your clinician, and keep it where you’ll see it. Your future self-calm, breathing easier-will thank you for it. Here’s your headline reminder to include on that page: bronchospasm action plan.




Harshitha Uppada
September 4, 2025 at 12:11
Life is a breath, but all we do is chase it like a dog after a ball, never stop to write down the map of our own lungs. It feels like a philosophical text written by a lazy student who never turned in the homework. If you were to even glance at the plan you might realize that the chaos you dread is just a chapter you skipped. Missin the plan is like forgetting to set your alarm before a big exam – you’ll wake up in panic.
So maybe grab a pen before the next wheeze, because “I’ll figure it out later” is just a fancy phrase for “I’ll die later.”