Managing medications at home isn’t just the patient’s job. For millions of older adults and people with chronic conditions, the real lifeline is the person sitting beside them-whether it’s a spouse, child, neighbor, or paid caregiver. Yet most families don’t know where to start. They’re told to "help with meds," but no one shows them how. The result? Missed doses, dangerous interactions, hospital trips, and sometimes worse. The good news? With the right system, you can cut medication errors by more than half and give everyone peace of mind.
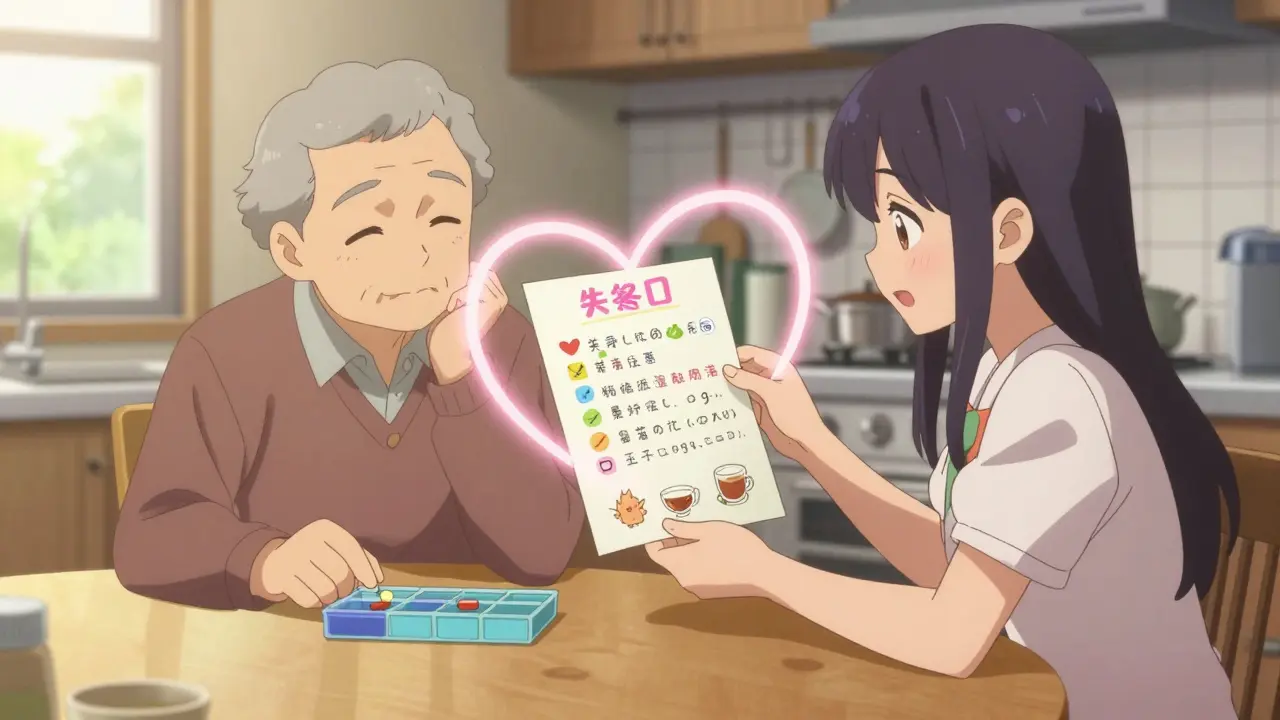
Start with a Complete Medication List
You can’t manage what you can’t see. The first step is building a master list of every medication the person takes. Not just the big ones. Not just the prescriptions. Everything. Including vitamins, supplements, over-the-counter painkillers, and even herbal teas that affect blood pressure. A full list needs these details for each item:- Brand name and generic name (e.g., "Lisinopril (Zestril)")
- Exact dosage (e.g., "10 mg", not "one pill")
- How often to take it (e.g., "once daily at 8 AM")
- When to take it (e.g., "with food," "on an empty stomach")
- Why it’s prescribed (e.g., "for high blood pressure")
- Prescribing doctor’s name and phone number
- Any known side effects or interactions
Use a Pill Organizer-But Choose the Right One
A simple 7-day pill box with morning and evening compartments reduces missed doses by 37%, according to a 2022 study in the Journal of the American Geriatrics Society. That’s not a small win. That’s the difference between staying out of the hospital and ending up there. But not all organizers work the same. If the person takes meds three or four times a day, get a 4-compartment box. If they’re forgetful or have memory issues, skip the manual box entirely. Go for an electronic dispenser like Hero Health or MedMinder. These devices lock and unlock compartments at the right time, flash lights, and send alerts to your phone if a dose is skipped. In clinical trials, they cut missed doses by 62%. And don’t forget refills. Set up automatic refills through CVS, Walgreens, or your Medicare Part D plan. Most pharmacies offer this now. You’ll get a text or email when it’s time to pick up, and you won’t run out because someone forgot to call.Build Routines Around Daily Habits
People remember routines better than alarms. That’s why linking meds to existing habits works so well. This is called "habit stacking," and it’s backed by the National Institute on Aging. Here’s how it works:- Take blood pressure pills right after brushing your teeth.
- Take diabetes meds before breakfast, while you’re waiting for your coffee to brew.
- Take nighttime pills after turning off the TV.
Use Technology-But Keep It Simple
Smartphones aren’t just for scrolling. Apps like Medisafe and Round Health send push notifications, track doses, and even alert family members if a dose is missed. In studies, users saw a 45% improvement in adherence compared to paper logs. If the person has trouble reading screens or using apps, try voice assistants. Amazon Alexa and Google Home can be set up to say, "It’s time for your heart pill," at 8 AM every day. A 2023 University of Pittsburgh study showed voice reminders reduced missed doses by 37% for people with dementia or cognitive decline. Don’t overcomplicate it. One app. One voice assistant. One reliable system. Too many tools create confusion. Pick one that works and stick with it.
Attend Appointments Together
Caregivers who go to doctor visits with their loved ones understand the medication plan 89% better, according to AARP’s 2023 Caregiving Survey. Why? Because doctors talk fast. They use jargon. They assume the patient remembers everything. Bring the medication list. Ask these four questions every time:- What time should this be taken relative to meals?
- Are there foods, drinks, or other meds I need to avoid?
- What should I do if a dose is missed?
- When should I expect to see results-or side effects?
Do Quarterly Medication Reviews
Medications change. Health changes. What worked last month might not work now. A quarterly review-every three months-isn’t optional. It’s essential. During the review, ask:- Are any pills no longer needed?
- Are any doses too high or too low?
- Is there a simpler way to take them? (e.g., one pill instead of three)
- Are there new side effects?
Prepare for Emergencies
Not all missed doses are equal. Missing a blood pressure pill? Maybe not urgent. Missing insulin? That’s a medical emergency. Create a "medication red list"-a separate card or note that says:- Insulin
- Blood thinners (like warfarin or apixaban)
- Heart medications (like digoxin or beta-blockers)
- Seizure meds
- Steroids (like prednisone)
Watch for the Big Risks
Polypharmacy-taking five or more medications-is common. About 45% of adults over 65 are on this many. And it’s dangerous. Each extra pill increases the chance of falls by 50% and hospitalization by 30%, according to Columbia University’s Dr. Barbara Guglielmo. Also watch for:- Changes in behavior (confusion, drowsiness, agitation)
- Unexplained bruising or bleeding
- Loss of appetite or sudden weight loss
- Falls or dizziness after a new med starts
Handle Transitions Carefully
The biggest danger spot? Going from hospital to home. That’s when 50-60% of medication errors happen, according to the Journal of General Internal Medicine. When your loved one is discharged:- Get a written discharge summary with the updated med list.
- Ask the nurse to walk through every change.
- Call the pharmacy to confirm all new prescriptions are filled correctly.
- Compare the hospital list to the old one. Did they stop something? Add something? Change the dose?
Don’t Burn Out
Medication management is exhausting. Forty-two percent of caregivers say it’s their most stressful task, according to the National Alliance for Caregiving. You’re not failing if you feel overwhelmed. You’re human. Ask for help. Can someone else refill prescriptions? Can a home care worker check doses? Can you use a pharmacy’s Medication Therapy Management (MTM) service? Medicare Part D offers this for free if the person takes eight or more drugs and has three or more chronic conditions. In 2023, 68% of eligible people used it. And remember: you’re not expected to be a pharmacist. You’re expected to be a team player. Work with the pharmacist, the doctor, the nurse. Let them do their job. You do yours: keep track, ask questions, and show up.What if my family member refuses to take their meds?
Don’t force it. First, find out why. Are they scared of side effects? Do they think it’s not working? Do they feel like it’s too many pills? Talk to their doctor. Sometimes switching to a once-daily pill or changing the medication helps. You can also use pill organizers with alarms or voice reminders to make it easier. If memory is the issue, consider a digital dispenser that locks doses until the right time. Never hide pills in food unless the doctor says it’s safe-some meds lose effectiveness or become dangerous when crushed.
Can I use a smartphone app even if my loved one doesn’t use one?
Absolutely. Apps like Medisafe let you set up reminders for someone else. You’ll get alerts when a dose is missed, and you can even notify other family members. Many caregivers use these to stay on top of meds for parents who live far away. You don’t need the person to use the phone-you just need access to your own.
What should I do if I find an old, unlabeled pill?
Don’t guess. Don’t throw it away. Take it to a pharmacy. Most pharmacists can identify unknown pills using a database based on color, shape, and imprint. Some even have machines that scan them. This is a common problem, especially after hospital stays or when multiple people live in the house. Getting it identified prevents accidental overdose or dangerous interactions.
Is it safe to cut pills in half to save money?
Only if the pill is scored and the doctor says it’s okay. Some pills, like extended-release tablets or capsules, can’t be split safely. Splitting them can cause the full dose to release at once, leading to overdose. Always check with the pharmacist before cutting any pill. If cost is an issue, ask about generic versions, patient assistance programs, or Medicare Part D cost-saving options.
How do I know if a medication is still needed?
Ask the doctor during every checkup. Many medications are started in the hospital and never reviewed again. The American Geriatrics Society’s Beers Criteria identifies drugs that are risky for older adults. If your loved one is on any of these, ask if they’re still necessary. Sometimes stopping a drug improves energy, balance, or appetite. Never stop a med cold turkey-always taper under medical supervision.




Sandeep Mishra
December 30, 2025 at 10:37
This is the kind of guide that should be handed out with every prescription. 🙏 I’ve seen my uncle go through 7 different meds in 3 months-no one told us what each one did, or when to take them. We just got a bag of pills and a shrug. Building that master list? Game-changer. I printed mine on cardstock and laminated it. Now it lives on the fridge next to the magnets. Simple, but it works.
And the red list? Genius. We added insulin and warfarin to ours. Last month, my aunt missed her dose and we called the doc before panic set in. Saved us a trip to ER. 🙌