NSAID Risk Calculator
Assess Your Risk
This tool calculates your personal risk of NSAID-related gastrointestinal bleeding based on your age, medical history, and medications. The American College of Gastroenterology recommends taking precautions for high-risk individuals.
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease a headache, back pain, or arthritic flare-up. These drugs - non-steroidal anti-inflammatory drugs, or NSAIDs - work fast and feel effective. But for many, especially older adults or those with existing health issues, what starts as a simple pain reliever can turn into a silent, life-threatening problem: gastrointestinal bleeding.
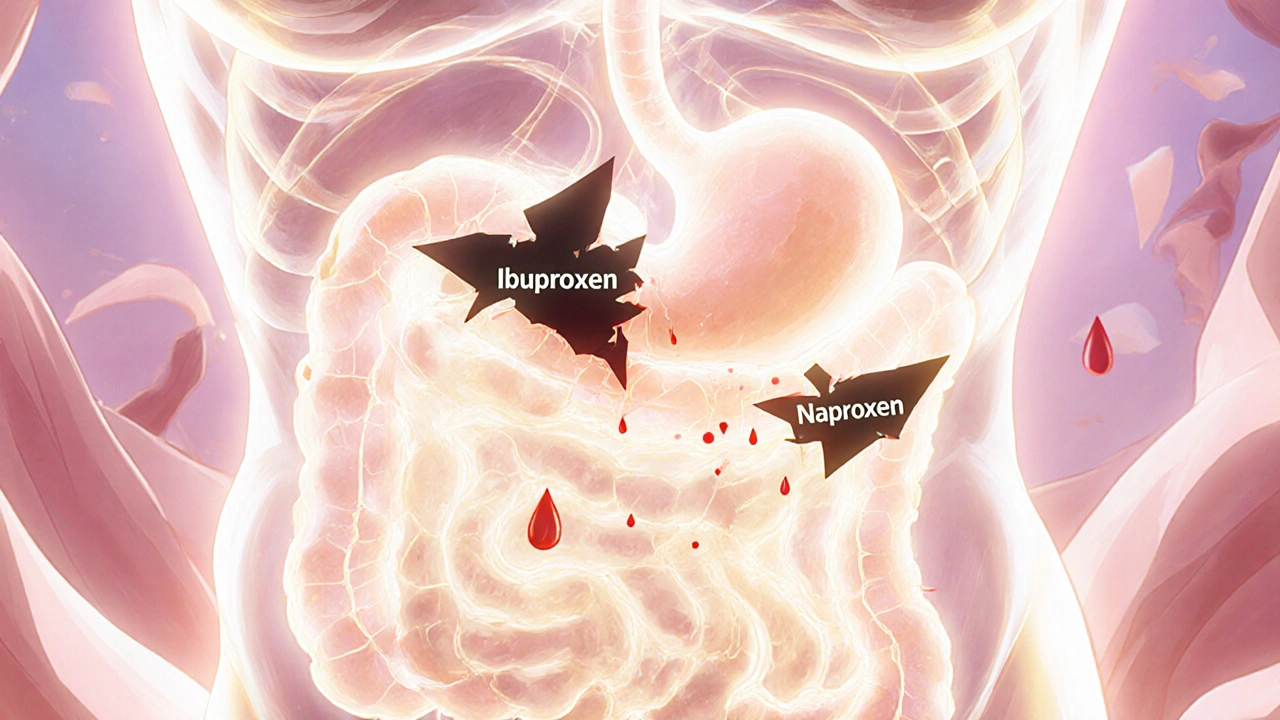
How NSAIDs Damage Your Stomach and Intestines
NSAIDs block enzymes called COX-1 and COX-2. COX-2 causes inflammation and pain, which is why these drugs help. But COX-1 protects your stomach lining by producing mucus and bicarbonate that shield it from acid. When COX-1 is blocked, that protection vanishes. Your stomach becomes vulnerable. Even a single dose can start causing tiny erosions. Over time, these turn into ulcers - open sores that can bleed without warning.It’s not just the stomach. Bleeding can happen anywhere in the GI tract - from the esophagus down to the small intestine. In fact, nearly one-third of NSAID-related bleeding cases originate below the stomach, according to the Cleveland Clinic Journal of Medicine. Many people never realize the source of their fatigue, dizziness, or pale skin is slow, hidden bleeding. That’s called occult bleeding, and it often leads to iron deficiency anemia before anyone connects it to their daily aspirin or Advil.
The Numbers Don’t Lie
The risk isn’t theoretical. A 2020 meta-analysis in JAMA Internal Medicine found that NSAID users are 3.2 to 4.2 times more likely to suffer upper GI bleeding or perforation than non-users. For someone over 65, that risk jumps even higher. And it’s not just prescription pills. Over-the-counter NSAIDs are a major contributor - 26% of users take more than the recommended dose, and most never tell their doctor.Some NSAIDs are riskier than others. Non-selective ones like naproxen and diclofenac carry the highest bleeding risk. Celecoxib, a COX-2 inhibitor, cuts that risk in half - but introduces a different danger: heart attacks. The 2004 APPROVe trial showed rofecoxib (a COX-2 drug) nearly doubled heart attack risk. That’s why celecoxib is still used, but only with caution.
Who’s Most at Risk?
Not everyone who takes NSAIDs will bleed. But certain factors stack the odds. The American College of Gastroenterology lists these key risk factors:- Age over 70 (risk doubles every decade)
- History of peptic ulcer or GI bleeding
- Use of blood thinners like warfarin or aspirin
- Taking corticosteroids (like prednisone)
- Using more than one NSAID at a time
- Chronic conditions like heart failure or kidney disease
If you have two or more of these, your risk isn’t just elevated - it’s critical. A 2019 study in the American Journal of Medicine found that patients with two or more risk factors have a 1 in 5 chance of developing a serious GI complication within a year of starting NSAIDs.
What Protects You?
The good news? There are proven ways to reduce the danger.Proton pump inhibitors (PPIs) - like omeprazole, esomeprazole, or pantoprazole - are the gold standard. A 2017 Cochrane review of over 13,000 patients showed PPIs reduce NSAID-related ulcers and bleeding by 75%. That’s not a small benefit. It’s life-saving. For high-risk patients, guidelines now say: start the PPI before the NSAID, not after symptoms appear.
Misoprostol is another option. It rebuilds stomach lining and cuts ulcer risk by 50-75%. But it causes diarrhea in up to 20% of users and isn’t safe during pregnancy. Most doctors avoid it unless PPIs aren’t an option.
Then there’s Vimovo, a new combo pill that pairs naproxen with esomeprazole. The 2022 PRECISION-2 trial showed it cut ulcer complications from 25.6% down to just 7.3% compared to naproxen alone. It’s not cheap, but for high-risk patients, it’s a game-changer.
Real People, Real Consequences
Behind the statistics are stories. On Reddit’s r/geriatrics, one user shared how their 78-year-old mother collapsed from internal bleeding. She’d been taking ibuprofen daily for knee pain. No one knew she was bleeding - until her hemoglobin dropped to 6.2 (normal is 12-16). She needed three blood transfusions.Another patient on HealthUnlocked said she felt constantly tired for months. Her doctor blamed stress. Only after her iron levels crashed did they find slow bleeding from an NSAID-induced ulcer. She’d been taking naproxen for 18 months.
But it’s not all bad news. On Drugs.com, 78% of users taking celecoxib reported no GI issues and effective pain control. The key difference? They were often prescribed it after a prior ulcer or with a PPI.

What Should You Do?
If you’re taking NSAIDs regularly, ask yourself:- Am I over 65?
- Have I ever had an ulcer or GI bleed?
- Am I on blood thinners or steroids?
- Am I taking more than one NSAID?
If you answered yes to two or more, talk to your doctor about switching to a safer option - like a COX-2 inhibitor with a PPI, or non-NSAID alternatives like acetaminophen or physical therapy.
Don’t assume OTC means safe. Just because you can buy it without a prescription doesn’t mean it’s harmless. The FDA has required black box warnings on all NSAID labels since 2005 - the strongest warning they give. That’s not a footnote. It’s a red flag.
For people with arthritis or chronic pain, NSAIDs may still be necessary. But they shouldn’t be automatic. The American College of Rheumatology now recommends using the lowest dose for the shortest time possible - especially if you have risk factors.
The Bigger Picture
NSAID-related GI bleeding causes about 107,000 hospitalizations and 16,500 deaths each year in the U.S. alone. The cost? Over $2.2 billion annually. That’s not just a medical problem - it’s a preventable public health crisis.And yet, many patients don’t know the risks. A 2022 survey by the Arthritis Foundation found that 42% of NSAID users stopped taking them because of stomach pain - but only 37% ever told their doctor. That silence kills.
There’s hope on the horizon. New drugs called CINODs - which combine NSAID action with nitric oxide to protect the gut - are in late-stage trials. Naproxcinod, for example, showed 50% fewer ulcers than naproxen in a 2021 study. But until they’re widely available, the tools we have - PPIs, COX-2 inhibitors, and awareness - are enough to save lives.
The bottom line? NSAIDs aren’t evil. They’re powerful. And like any powerful tool, they need respect. If you’re using them long-term, don’t wait for symptoms. Ask your doctor: “Am I at risk for bleeding? Do I need a protective medication?” That conversation could be the difference between relief and a hospital bed.
Can I take NSAIDs if I’ve had a peptic ulcer before?
If you’ve had a peptic ulcer or GI bleeding before, NSAIDs are generally not recommended unless absolutely necessary. If you must take them, guidelines strongly recommend combining a COX-2 inhibitor like celecoxib with a proton pump inhibitor (PPI). This combination reduces the risk of another ulcer by up to 80%. Never restart NSAIDs after a bleed without discussing it with a gastroenterologist.
Do all NSAIDs cause the same level of bleeding risk?
No. Non-selective NSAIDs like naproxen, diclofenac, and high-dose ibuprofen carry the highest risk because they block both COX-1 and COX-2. Selective COX-2 inhibitors like celecoxib cause significantly less stomach damage - about half the rate of ulcers and bleeding. However, COX-2 inhibitors carry higher cardiovascular risks, so the choice depends on your individual health profile.
Can over-the-counter NSAIDs cause serious bleeding?
Absolutely. Many people assume OTC means safe, but that’s a dangerous myth. Studies show that 26% of people take OTC NSAIDs at doses higher than recommended, and most don’t tell their doctor. Bleeding can happen even with short-term use in high-risk individuals. A 2021 review found that nearly half of all NSAID-related GI bleeds occur in people taking over-the-counter doses.
How do I know if NSAIDs are causing internal bleeding?
Signs can be subtle. Watch for fatigue, dizziness, pale skin, or shortness of breath - these may point to anemia from slow bleeding. Dark, tarry stools (melena) or vomiting blood are clear red flags. But many people don’t notice anything until they’re severely anemic. If you’re on NSAIDs long-term, ask your doctor for a simple blood test to check your hemoglobin and iron levels once a year.
Are there alternatives to NSAIDs for pain relief?
Yes. For mild to moderate pain, acetaminophen (Tylenol) is safer for the stomach. For arthritis, topical NSAID gels or creams deliver pain relief with far less systemic absorption. Physical therapy, weight management, and heat/cold therapy can also reduce reliance on pills. In some cases, doctors may prescribe duloxetine or pregabalin for nerve-related pain. Always discuss alternatives - especially if you have risk factors for bleeding.
Should I take a PPI if I’m on NSAIDs but have no symptoms?
If you have two or more risk factors - like age over 70, history of ulcer, or use of blood thinners - yes. Guidelines recommend starting a PPI at the same time as the NSAID, even if you feel fine. Bleeding often happens without warning. Preventing it is far easier than treating it. For low-risk users taking NSAIDs occasionally, PPIs aren’t usually needed.



Aki Jones
November 25, 2025 at 14:41
So let me get this straight: the FDA has had a BLACK BOX warning on NSAIDs since 2005… and yet, every pharmacy shelf is flooded with them like they’re candy? Someone’s making billions off people’s ignorance-and it’s not the doctors. This isn’t negligence. It’s systemic exploitation. The pharmaceutical lobby owns Congress, and your stomach lining? That’s just collateral damage in the profit calculus. You think they care about your anemia? No. They care about your next refill.