Hyponatremia Risk Calculator for Older Adults
Check Your Risk
This tool estimates your risk of hyponatremia when taking SSRIs based on key factors from medical research. It's designed for adults over 65.
Why SSRIs Are Risky for Older Adults
More than 1 in 5 Americans over 65 are taking SSRIs - antidepressants like sertraline, fluoxetine, and escitalopram - to manage depression or anxiety. But for older adults, these medications come with hidden dangers that aren’t always obvious. One of the most serious risks is hyponatremia: dangerously low sodium levels in the blood. It’s not rare. About 6 out of every 100 older adults on SSRIs develop it, and for some, it leads to confusion, dizziness, falls, and even hospitalization.
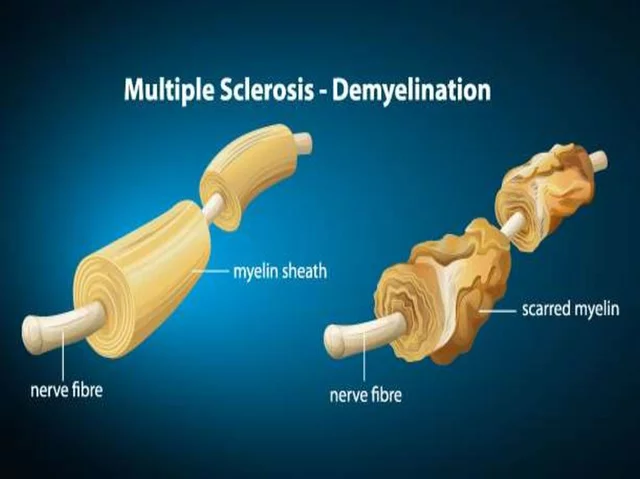
The problem isn’t the depression itself - it’s how the body changes with age. As we get older, our kidneys don’t work as well. We have less total body water. Our hormones that control fluid balance, like antidiuretic hormone (ADH), start misfiring. SSRIs make this worse by triggering something called SIADH - where the body holds onto too much water, diluting the sodium in your blood. The result? Sodium drops below 135 mmol/L, and symptoms creep in quietly: fatigue, stumbling when walking, feeling foggy, or just not feeling like yourself.
Who’s Most at Risk?
Not every older adult on SSRIs will get hyponatremia, but some are far more likely. Women are at higher risk. People with a low body weight (BMI under 25) are more vulnerable. Those with already low sodium levels - even just a little below normal - are in danger. And if you’re taking a thiazide diuretic for high blood pressure? That’s a red flag. The combination of a diuretic and an SSRI increases your risk by more than 20%.
Some SSRIs are riskier than others. Fluoxetine (Prozac) has the highest reported rate of hyponatremia among this class - nearly 6.5% of users. Sertraline and citalopram follow close behind. Venlafaxine, an SNRI often used instead of SSRIs, carries a similar risk. On the other hand, mirtazapine and bupropion show much lower rates of sodium problems. That’s not just a footnote - it’s a decision point.
The Silent Link Between Low Sodium and Falls
Hyponatremia doesn’t always cause nausea or seizures. In older adults, it often just makes you unsteady. You might not feel dizzy. You might not realize your balance is off. But your gait changes. Your steps become shorter. Your feet drag. You lean to one side. These subtle shifts are why hyponatremia is so strongly tied to falls - and why falls are the leading cause of injury and death in seniors.
There’s no direct study that says, “SSRI-induced hyponatremia causes 40% of falls in elderly patients.” But if you look at the patterns - the dizziness, the confusion, the weakness - they match exactly what happens when sodium drops. And when a senior falls, the consequences are brutal: hip fractures, brain bleeds, long-term disability, loss of independence. One study at Johns Hopkins found that patients with untreated mild hyponatremia were three times more likely to fall within three months. That’s not coincidence. It’s cause and effect.
What Doctors Should Do - and What They Often Don’t
Guidelines from the American Geriatrics Society and JAMA Internal Medicine are clear: check sodium levels before starting an SSRI, and check again within two weeks. Simple blood test. Takes five minutes. Costs less than $20. Yet, a 2023 study found that only 37% of geriatricians consistently follow this rule. Why? Busy clinics. No automated alerts. Staff shortages. And a false belief that “if the patient feels fine, there’s no problem.”
Here’s the hard truth: 30-40% of people with hyponatremia have no symptoms at all. You can’t wait for someone to say, “I feel weird.” By then, it might be too late. That’s why routine testing isn’t optional - it’s essential. The American Society of Health-System Pharmacists created a decision tool used in over 120 hospitals that flags high-risk combinations (like SSRI + hydrochlorothiazide) and auto-sends a lab order. Hospitals using it reduced dangerous prescribing by nearly 20%.
What You Can Do - Even If You’re Not a Doctor
If you or a loved one is on an SSRI, here’s what to ask for and watch for:
- Ask for a baseline sodium test before the first pill is taken.
- Request a repeat test two weeks after starting - or after any dose increase.
- Review all medications with your pharmacist. Are you on a water pill? A blood pressure med? A painkiller? Many interact with SSRIs.
- Watch for subtle signs: stumbling on level ground, needing to hold onto walls, feeling unusually tired, or having trouble remembering simple things.
- Ask about alternatives. Is mirtazapine or bupropion a better fit? Psychotherapy? Both have proven benefits with far less risk.
Don’t assume your doctor knows all this. Many don’t. Bring this information with you. Write down your questions. Be the advocate.

When to Switch Medications
If your sodium level drops below 130 mmol/L, stopping the SSRI is usually the first step. Mild cases (125-134) often improve with fluid restriction and close monitoring. Severe cases (below 125) need hospital care - but correction must be slow. Too much sodium too fast can cause brain damage.
For long-term treatment, consider switching to a safer antidepressant. Mirtazapine is the top choice for older adults with hyponatremia risk. It doesn’t affect ADH. It doesn’t cause fluid retention. It’s effective for depression and even helps with sleep and appetite - two common problems in seniors. Bupropion is another option, though it’s less helpful for anxiety. Neither is perfect, but both are much safer than fluoxetine or sertraline in this population.
The Bigger Picture: Why This Is Getting Worse
SSRI prescriptions for seniors have jumped 34% since 2015. More people are being diagnosed with depression. More doctors are prescribing antidepressants instead of therapy. But the safety infrastructure hasn’t kept up. The FDA added stronger warnings in 2022, but they’re buried in fine print. Medicare spends $1.2 billion a year treating hyponatremia-related hospitalizations - money that could be saved with simple blood tests.
New tools are emerging. A $2.8 million NIH study launched in September 2024 is testing AI models that predict who’s most likely to develop hyponatremia based on age, meds, sodium trends, and fall history. Some clinics are already using smart alerts that pop up when a doctor tries to prescribe an SSRI to someone on a diuretic. But until these become standard, the burden falls on patients and families.
Final Thought: It’s Not About Avoiding Antidepressants - It’s About Choosing Wisely
Depression in older adults is real. Untreated, it kills. But SSRIs aren’t the only answer. And for many, they’re the wrong one. The goal isn’t to stop treatment - it’s to start it safely. A simple blood test. A conversation about alternatives. A watchful eye on walking patterns. These aren’t big steps. But they can mean the difference between staying independent and ending up in the hospital - or worse.
If you’re taking an SSRI and you’ve had a fall, or you feel unsteady, don’t wait. Ask for your sodium level. Ask about other options. Your balance - and your future - depends on it.
Can SSRIs cause falls in older adults?
Yes. SSRIs don’t directly cause falls, but they can lead to hyponatremia - low sodium levels - which causes dizziness, confusion, and poor balance. These symptoms increase fall risk significantly in older adults. Studies show a strong link between SSRI use and falls, especially when sodium levels drop below 130 mmol/L.
How do I know if I have hyponatremia from SSRIs?
You often won’t feel anything at first. Early signs are subtle: stumbling on flat ground, feeling unusually tired, having trouble concentrating, or noticing your balance isn’t what it used to be. The only reliable way to know is through a blood test. If you’re on an SSRI and you’re over 65, ask your doctor for a serum sodium test - especially within the first two weeks of starting the medication.
Which SSRI is safest for older adults?
Fluoxetine (Prozac) carries the highest risk of hyponatremia. Safer alternatives include mirtazapine and bupropion. Mirtazapine has minimal impact on sodium levels and is often better tolerated in seniors. It also helps with sleep and appetite, which are common issues. Always discuss alternatives with your doctor - the best choice depends on your symptoms, other meds, and health history.
Should I stop taking my SSRI if I’m worried about hyponatremia?
Don’t stop abruptly. Stopping SSRIs suddenly can cause withdrawal symptoms like anxiety, nausea, or brain zaps. Instead, talk to your doctor. Get a sodium test. If your levels are low, your doctor can help you taper off safely and switch to a lower-risk medication. Monitoring and switching are safer than stopping on your own.
Can I prevent hyponatremia without stopping my medication?
Yes - but only with medical supervision. You can reduce risk by avoiding excessive water intake, reviewing all medications with your pharmacist (especially diuretics), and getting regular sodium tests. But if your sodium drops below 130 mmol/L, you’ll likely need to change your antidepressant. Prevention means catching it early - not waiting for symptoms.




Dana Dolan
November 20, 2025 at 19:13
I had no idea SSRIs could mess with sodium like this. My mom’s on sertraline and lately she’s been stumbling a bit - I thought it was just aging. Guess I’m calling her doctor tomorrow. Thanks for the wake-up call.