Introduction to Prednisolone and Prednisone
As a health-conscious individual, it's essential to understand the differences between two commonly prescribed medications: Prednisolone and Prednisone. These two drugs are often used interchangeably, but they have some key differences that can affect their efficacy and side effects. In this article, I will explore these differences in detail, so you can make an informed decision about which medication is right for you.
Understanding the Basics: What Are Prednisolone and Prednisone?
Before delving into the differences, let's first understand what these medications are. Prednisolone and Prednisone are both corticosteroids, which are a class of synthetic steroid hormones that mimic the effects of cortisol, a naturally occurring hormone produced by the adrenal glands. Corticosteroids have anti-inflammatory, immunosuppressive, and anti-allergic effects, making them useful for treating a wide range of conditions, such as asthma, allergies, and autoimmune disorders.
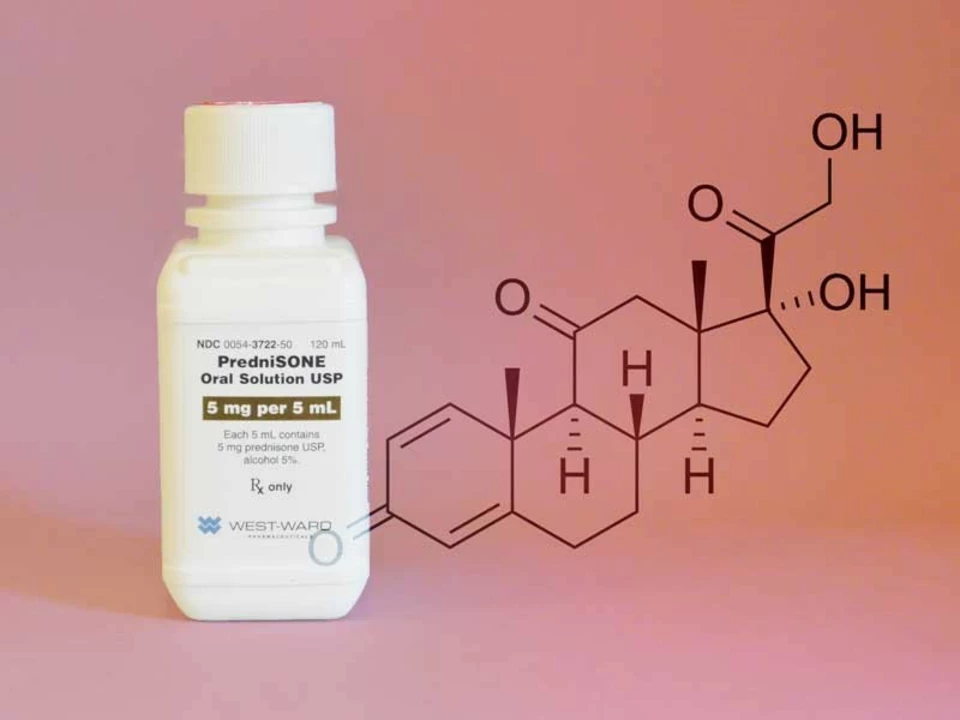
The Chemistry Behind the Medications: Prednisolone vs. Prednisone
The primary difference between Prednisolone and Prednisone lies in their chemical structure. Although both are corticosteroids, Prednisone is a prodrug, meaning it needs to be metabolized by the liver to convert into its active form, Prednisolone. On the other hand, Prednisolone is already in an active form and can be directly utilized by the body.
How Does This Chemical Difference Affect the Potency of the Drugs?
Because Prednisone needs to be converted into Prednisolone, its effectiveness can vary depending on the individual's liver function. For people with healthy liver function, this conversion happens efficiently, and the potency of the two drugs is relatively similar. However, for those with impaired liver function, the conversion may be less effective, which means Prednisolone might be a better option, as it does not require this conversion process.
Comparing the Side Effects: Which Drug Has Fewer Side Effects?
Both Prednisolone and Prednisone can cause similar side effects, as they belong to the same class of medications. These side effects can include fluid retention, weight gain, high blood pressure, mood changes, and increased risk of infections. However, because Prednisone needs to be metabolized by the liver, it may cause additional side effects related to liver function, especially in people with pre-existing liver conditions. Therefore, Prednisolone might be a safer option in such cases.
Drug Interactions: How Do Prednisolone and Prednisone Interact with Other Medications?
Both Prednisolone and Prednisone can interact with other medications, and it's essential to discuss your current medications with your healthcare provider before starting either drug. Some common drug interactions include anticoagulants, antifungal medications, and certain antibiotics. While the interaction profiles of both drugs are quite similar, there might be some differences in how they interact with other medications, depending on the specific drug and the individual's unique metabolism.
Dosage and Administration: How Are Prednisolone and Prednisone Taken?
Both Prednisolone and Prednisone are available in various forms, including tablets, oral solutions, and injections. The dosages vary depending on the condition being treated and the individual's specific needs. Because Prednisone needs to be converted into Prednisolone in the body, the dosages may not be directly interchangeable. It's crucial to follow your healthcare provider's instructions carefully and never adjust your dosage without consulting them first.
Cost and Availability: Is One Drug More Affordable or Accessible Than the Other?
In general, both Prednisolone and Prednisone are widely available and relatively affordable. However, the cost may vary depending on factors like the specific formulation, the brand, and your location. It's essential to compare prices and availability in your area to determine which medication might be the more cost-effective option for you.
Effectiveness and Patient Preference: Which Drug Do Patients Prefer?
As mentioned earlier, the effectiveness of Prednisolone and Prednisone can be quite similar for individuals with healthy liver function. However, some patients might prefer one drug over the other based on factors like side effects, drug interactions, or personal experience. It's essential to discuss your preferences and concerns with your healthcare provider, who can help you decide which medication is the best fit for you and your unique needs.
Final Thoughts: Making the Right Choice for You
Ultimately, the choice between Prednisolone and Prednisone depends on your individual circumstances, medical history, and preferences. While both medications have their benefits and drawbacks, understanding their differences can help you make an informed decision about your treatment plan. Always consult your healthcare provider before making any changes to your medications, and remember that the best treatment approach is one tailored to your unique needs and circumstances.




Joseph Bowman
June 12, 2023 at 13:02
Hey there, just a heads‑up that the pharma giants don’t want us to notice the subtle differences between prednisolone and prednisone. They push both on the shelves so we stay confused, while the real chemistry gets hidden behind glossy labels. The fact that prednisone needs a liver conversion is a perfect way to keep the supply chain complex and profitable. If you have any liver issues, you might be silently paying for a “premium” version without even knowing it. Stay vigilant, friends, and always ask your doctor to spell out why they chose one over the other.