The Rising Concern of Fatty Liver Disease
Fatty liver disease, particularly non-alcoholic fatty liver disease (NAFLD), is becoming an increasingly prevalent health concern around the globe. NAFLD, characterized by excess fat stored in liver cells not due to alcohol consumption, affects millions and can lead to severe health complications, including cirrhosis and liver cancer. The absence of FDA-approved medications specifically for NAFLD has left a significant gap in effective treatment, highlighting the urgency for new therapeutic options.
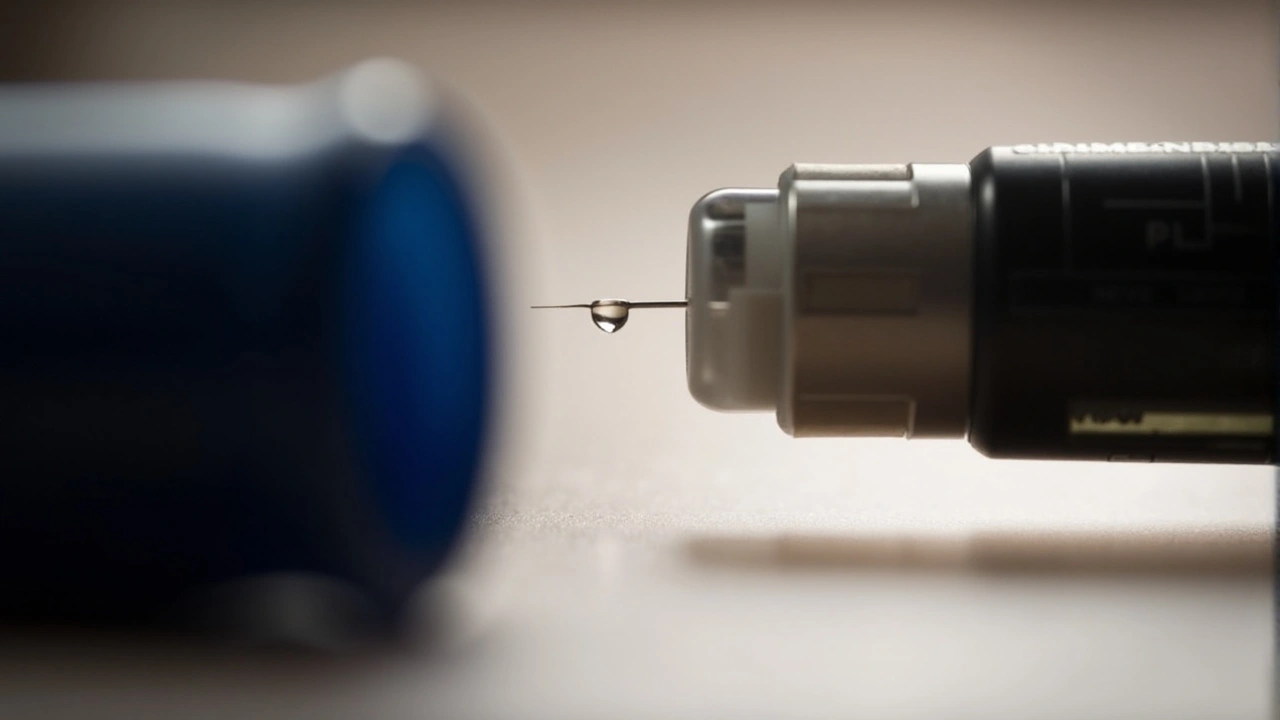
Understanding Semaglutide
Semaglutide, a prescription medication primarily used to manage type 2 diabetes, could be a game-changer in this regard. It belongs to the class of glucagon-like peptide-1 (GLP-1) receptor agonists. These medications work by delaying stomach emptying, inhibiting the release of glucagon, and promoting the function of pancreatic beta cells that produce and release insulin. The drug is marketed under names like Ozempic, Rybelsus, and Wegovy, with each serving slightly different purposes but stemming from the same active ingredient, semaglutide.
The Weight Loss Connection
In addition to its benefits for diabetes, semaglutide is effective in promoting weight loss. This effect is particularly noteworthy as obesity is a major risk factor for developing NAFLD. By aiding in weight loss, semaglutide indirectly contributes to better liver health. More importantly, research indicates that semaglutide may directly benefit the liver by reducing fat content, a crucial factor in managing NAFLD.
Research and Findings
Several studies have shown promising results regarding the use of semaglutide for NAFLD. One study involving 458 participants—321 of whom received semaglutide and 137 a placebo—demonstrated that semaglutide effectively improved liver health markers with low rates of side effects. Another study highlighted that a 24-week regimen of semaglutide significantly improved liver enzyme levels, a key indicator of liver health, in individuals with NAFLD or non-alcoholic steatohepatitis (NASH).
Mechanism of Action
So how does semaglutide achieve these benefits? The drug enhances blood sugar control, which is crucial for liver health, and promotes weight loss, which directly reduces liver fat. Additionally, semaglutide exhibits antioxidant and anti-inflammatory properties that further support liver health. These combined actions make it a multifaceted tool in managing NAFLD, even though it is not yet FDA-approved for this specific condition.
Potential Therapeutic Implications
The findings so far suggest that semaglutide might fill a significant treatment gap for people suffering from NAFLD. While more research and clinical trials are necessary to confirm its efficacy and safety for this particular use, the initial results are promising. This could mean a significant shift in how NAFLD is managed, offering hope for patients who currently rely mostly on lifestyle changes for managing their condition.
Lifestyle Changes and NAFLD
For most individuals, lifestyle changes remain the frontline defense against NAFLD. Regular exercise, a balanced diet, and minimizing alcohol intake are strongly recommended. Medications to lower cholesterol and triglyceride levels are often prescribed in more severe cases. However, the potential of semaglutide to complement these lifestyle changes and offer an alternative treatment method is a significant development.
Ozempic and Wegovy
Ozempic and Wegovy, both containing semaglutide, are often prescribed for their beneficial effects on weight loss. While Ozempic is sometimes used off-label for this purpose, Wegovy is FDA-approved for weight management. The use of these medications should always be discussed in detail with healthcare providers to weigh potential risks and benefits.
The Road Ahead
As the research community continues to explore semaglutide's full potential, its possible application in treating NAFLD seems increasingly feasible. This could revolutionize the treatment landscape, providing effective options for those at risk of severe liver disease. In the meantime, individuals suffering from NAFLD should continue to focus on proven lifestyle modifications while staying informed about emerging therapies.
Conclusion
Semaglutide stands at the frontier of a potentially groundbreaking approach to managing NAFLD. Despite not being FDA-approved specifically for liver disease, its significant impact on weight loss, blood sugar control, and liver health markers holds much promise. With ongoing research, semaglutide may soon become a cornerstone treatment for individuals grappling with fatty liver disease.





Derrick Blount
August 17, 2024 at 18:44
The advent of semaglutide in the therapeutic arsenal invites a profound reexamination of metabolic pathophysiology. One must first acknowledge that the drug’s GLP‑1 agonism operates not merely as a glycaemic regulator, but as a pleiotropic modulator of hepatic lipid homeostasis. Empirical evidence, as presented in recent double‑blind trials, demonstrates a statistically significant attenuation of hepatic steatosis indices among subjects receiving semaglutide. Moreover, the pharmacokinetic profile of semaglutide, characterized by a prolonged half‑life, ensures sustained receptor activation, thereby mitigating post‑prandial insulin spikes. This sustained activation, in turn, curtails de novo lipogenesis, a principal driver of intra‑hepatic fat accumulation. Simultaneously, the medication’s effect on satiety hormones engenders a caloric deficit that further potentiates adipose tissue mobilization. It is imperative, however, to distinguish correlation from causation when interpreting reductions in alanine aminotransferase levels. While lowered enzyme concentrations are encouraging, they may reflect ancillary improvements in systemic inflammation rather than direct hepatic regeneration. Consequently, mechanistic studies employing hepatic biopsy endpoints are indispensable for elucidating the true histological impact. The safety profile, albeit favorable, is not devoid of adverse events; nausea, vomiting, and rare pancreatitis remain documented. Clinicians must therefore balance therapeutic optimism with vigilant monitoring, especially in patients with pre‑existing pancreatic risk factors. Ethical considerations also arise when prescribing off‑label for non‑alcoholic fatty liver disease, given the current FDA stance. From a health‑economics perspective, the cost‑effectiveness of semaglutide hinges upon its long‑term outcomes, which remain to be fully quantified. Nevertheless, the convergence of weight loss, glycaemic control, and hepatic benefit positions semaglutide as a unique candidate for multimodal intervention. Future randomized controlled trials should stratify participants by baseline fibrosis stage to assess differential efficacy. In sum, while enthusiasm is justified, rigorous scientific validation will ultimately determine whether semaglutide reshapes the therapeutic landscape of NAFLD.