Every year, Americans fill over 6 billion prescriptions. About 92% of those are for generic drugs. That’s a huge win for cost savings - over $313 billion in annual savings. But here’s the thing: whether you get a generic version of your prescription depends not on federal law, but on state laws. And those laws? They’re wildly different from one state to the next.
Why State Laws Matter
You might think the FDA sets the rules for generic drugs. And yes, the FDA approves them. But when it comes to whether your pharmacist can swap your brand-name drug for a generic - that’s up to your state. All 50 states and Washington, D.C. have their own rules. Some are strict. Some are loose. Some require you to say yes. Others assume you’re okay unless you say no.This patchwork system affects real people. A pharmacist in Texas might automatically substitute a generic statin. But in Hawaii, they can’t swap an antiepileptic drug without getting both the doctor’s and the patient’s permission. That’s not a typo. It’s the law.
Four Key Ways States Differ
State laws on generic substitution boil down to four big differences:
- Do pharmacists have to substitute? In 22 states, yes - they’re legally required to swap in a generic unless the doctor or patient blocks it. In the other 28 states and D.C., they can choose to substitute, but they don’t have to.
- Do you need to give permission? In 32 states, the law assumes you’re okay with substitution unless you say otherwise. That’s called presumed consent. In 18 states, you must actively say yes - explicit consent. No signature? No swap.
- Do you get notified? Forty-one states require the pharmacist to tell you after they make the switch. That means a phone call, a note on your receipt, or a pop-up on the pharmacy screen. But in nine states? No notice required.
- Are pharmacists protected? In 37 states, if a pharmacist follows the rules, they’re shielded from lawsuits or criminal charges if something goes wrong. In the other 13? They could be on the hook.
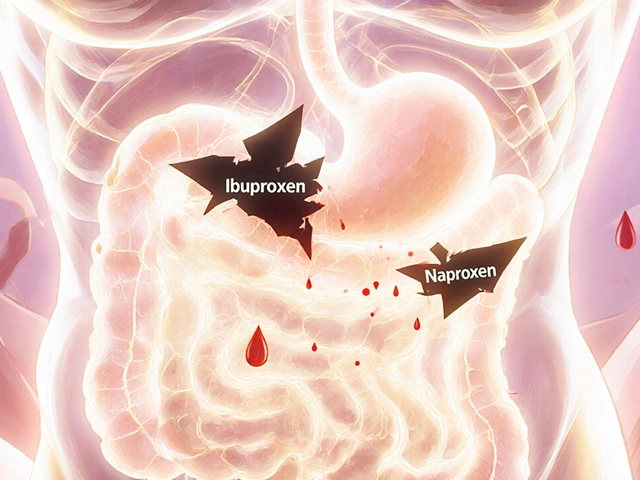
What About Dangerous Drugs?
Not all drugs are created equal. Some have a narrow therapeutic index (NTI). That means the difference between a dose that works and one that’s dangerous is tiny. Warfarin. Levothyroxine. Some epilepsy drugs. Even if the FDA says a generic is equivalent, real-world problems happen.
Minnesota had a case where a patient switched from brand-name warfarin to a generic and ended up with a dangerous blood clot. The FDA’s own adverse event reports show 53 reports of problems with warfarin substitutions between 2020 and 2022. Another 89 involved levothyroxine.
So 15 states - including Kentucky, Ohio, and New York - have special lists. They block substitution for certain NTI drugs. Kentucky’s list includes digitalis glycosides and antiepileptics. In Hawaii, even if a drug isn’t on the list, you still need both doctor and patient approval to switch an epilepsy medication.
How It Plays Out in Real Life
Imagine you live in New York. You pick up your prescription. The pharmacist asks, “Do you want the generic?” You say yes. Next week, you move to New Jersey. You go to the same pharmacy chain. No questions asked. The generic is automatically swapped. You’re confused. Your friend who lives in Oklahoma? They can’t get a generic unless the doctor writes “dispense as written.”
That’s not hypothetical. A 2022 survey of 1,200 independent pharmacists found that 78% of them get confused by the rules when handling prescriptions from other states. And 18% of chain pharmacy transactions involve prescriptions crossing state lines.
Patients notice, too. Reddit threads are full of stories: “I got the brand again because I thought I was supposed to ask. Turns out I didn’t need to.” Or, “My doctor told me not to switch, but the pharmacy did anyway.”
What’s the Impact?
It’s not just about confusion. It’s about money and health.
States with mandatory substitution have generic fill rates of 94.1%. States with permissive rules? Only 88.3%. That’s a 6-point gap - billions of dollars in savings. One study found mandatory substitution saved Medicaid programs $1.2 billion a year.
But there’s a flip side. A 2023 report from the Life Raft Group found that 41% of cancer patients worry about substitution for NTI drugs. And 28% of them have been told by their doctors to refuse generics outright.
Pharmacists spend over 12 minutes per prescription checking state rules, drug lists, and patient history. That’s time they could spend counseling patients. Most pharmacies now use software that auto-checks state laws - and it cuts errors by 64%.

The Big Picture
There’s no national standard. The FDA says generics are safe. The American Pharmacists Association says we need one set of rules. But states aren’t budging. Why? Because they’re responding to local concerns - cost control vs. patient safety.
Some states, like Louisiana, are super favorable to substitution. Others, like Hawaii, are the most restrictive. Oklahoma? It’s an outlier. Florida requires each pharmacy to create its own formulary. Iowa says stick to the FDA’s Orange Book.
And now, with biosimilars - the next generation of complex generic drugs - things are getting even messier. As of 2023, 49 states have rules for biosimilar substitution. But each one is different. Hawaii still requires dual consent for epilepsy drugs. Florida has its own safety formulary. And 12 states updated their laws in 2023 to match the FDA’s new “interchangeable” designation.
The Congressional Budget Office estimates that if all states aligned their rules, we could save another $8.7 billion by 2028. But patient advocacy groups warn: too much standardization could put lives at risk.
What You Should Do
Here’s the practical advice:
- Ask your pharmacist: “Can you substitute this drug? What does your state allow?”
- If you’re on a narrow therapeutic index drug - like warfarin, levothyroxine, or an antiepileptic - ask your doctor to write “dispense as written” on the prescription.
- Check your receipt. If the drug changed, you should see a note. If you don’t, ask.
- If you move to a new state, update your pharmacy. Rules change.
There’s no magic fix. The system is messy. But understanding your state’s rules - and speaking up - gives you control over your care.
Can my pharmacist substitute a generic drug without telling me?
In 9 states, yes - they’re not required to notify you. But in 41 states, they must. Even if they don’t tell you, you have the right to ask. Always check your prescription label and receipt. If the drug name changed, it was substituted.
Why can’t I get a generic for my seizure medication?
Because your state may have special rules for narrow therapeutic index (NTI) drugs. Drugs like levetiracetam or phenytoin have very tight safety margins. Even small differences in absorption can cause seizures or toxicity. Fifteen states, including Kentucky and New York, ban substitution for these drugs. Others require explicit patient consent.
Is a generic drug really the same as the brand name?
For most drugs, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration. They must also be absorbed at the same rate and amount. But for NTI drugs, some patients report differences - even when the FDA says they’re equivalent. That’s why doctors sometimes write “dispense as written.”
What’s the Orange Book, and why does it matter?
The FDA’s Orange Book lists all approved generic drugs and their therapeutic equivalence ratings. Drugs rated “A” are considered interchangeable. “B” means they’re not. All 50 states use the Orange Book as their baseline. But 15 states add their own lists of drugs that can’t be substituted, even if they’re rated “A.”
Can I refuse a generic even if my state allows automatic substitution?
Yes. Every state allows patients to refuse substitution. You don’t need a doctor’s note. Just tell the pharmacist: “I want the brand.” They must honor it. Some states even require them to ask you. If they don’t, ask again. Your right to choose your medication is protected.
Why do some states require patient consent and others don’t?
It’s a trade-off between cost and control. States with presumed consent (like California and Texas) prioritize savings - they assume most people want the cheaper option. States with explicit consent (like New Jersey and Maryland) prioritize patient autonomy. They believe you should actively agree to a change, especially if you’re on a sensitive medication.