Analgesic basics: pick the right pain reliever for the job
Pain isn’t one-size-fits-all. A sore muscle after yard work needs a different approach than burning nerve pain or a bad migraine. Knowing the main types of analgesics and when to use them helps you feel better faster and avoid common risks.
How to choose an analgesic
Start by matching the medicine to the pain type. For mild to moderate, short-term pain (headache, fever, muscle ache): acetaminophen (paracetamol) or an NSAID usually works well. NSAIDs—like ibuprofen or naproxen—cut inflammation and swelling. Acetaminophen eases pain and lowers fever but doesn’t reduce inflammation.
For inflammatory pain (sprains, arthritis flare-ups), NSAIDs are often better because they target the inflammation causing the pain. For neuropathic pain (burning, tingling, shooting pains), antidepressants (like certain SNRIs) or anticonvulsants (gabapentin) can be more effective than standard analgesics.
Topical analgesics—gels, creams, or patches containing NSAIDs, lidocaine, or capsaicin—work well for localized aches and cut systemic side effects. Stronger prescription options, including short-course opioids, are sometimes used for severe acute pain after surgery or major injury. Those carry higher risk and should be used only under clear medical guidance.
Safety tips & when to see a doctor
Know the common risks. NSAIDs can irritate the stomach, raise blood pressure, and affect kidney function—especially if you already have heart or kidney disease or take blood thinners. Acetaminophen is easier on the stomach but can harm the liver if you exceed safe doses—don’t mix several products that both contain acetaminophen.
Simple rules to lower risk: follow the dosing on the label, use the lowest effective dose for the shortest time, and tell your doctor about all other medicines you take, including supplements. Avoid alcohol while using acetaminophen or when taking opioids. If you’re pregnant, breastfeeding, or have chronic conditions (liver, kidney, heart disease), check with your clinician before using any analgesic.
Watch for red flags: severe or worsening pain, new fever, numbness or weakness, sudden shortness of breath, or signs of allergic reaction (rash, swelling). If those happen, get medical help right away.
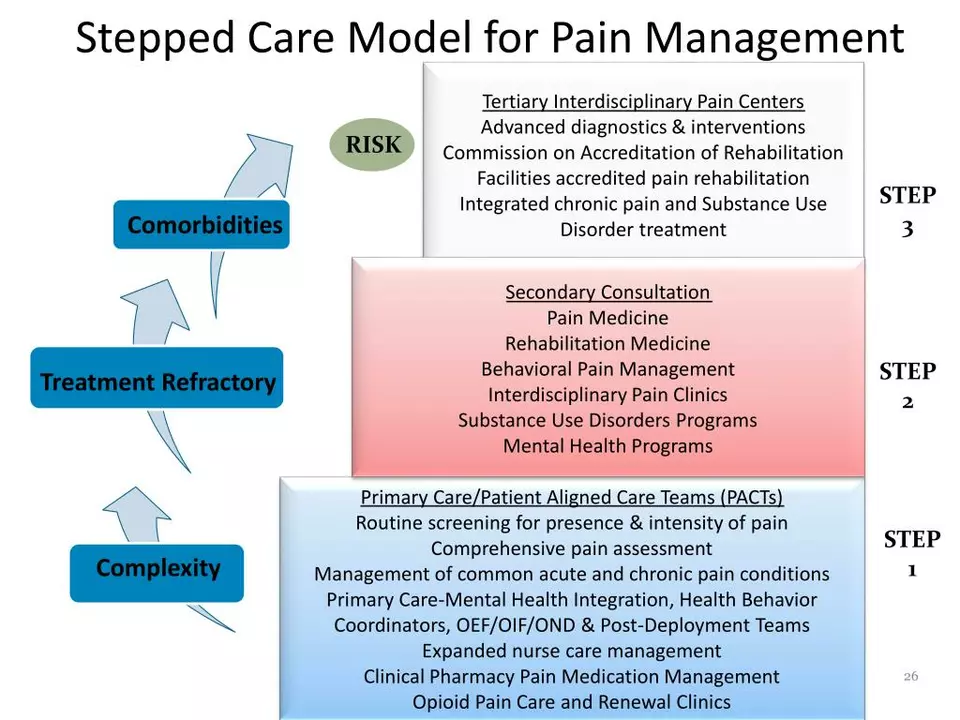
Non-drug options matter too. Rest, ice or heat, gentle stretching, physical therapy, and targeted exercise can reduce pain and lower your need for medicine. For chronic pain, combining meds with therapy, exercise, and sleep improvement often works best.
If you’re unsure which analgesic fits your pain, send a quick message to your healthcare provider or pharmacist. A short conversation can help you pick a safer, more effective option and avoid common mistakes.
The Role of Ketorolac in Pain Management
In my latest blog post, I explored the role of Ketorolac in pain management. Ketorolac is a nonsteroidal anti-inflammatory drug (NSAID) that is commonly used for short-term pain relief. I discovered that it's particularly effective in treating moderate to severe acute pain, often following surgery. However, it's important to note that Ketorolac should be used cautiously, as it can cause serious side effects such as gastrointestinal bleeding and kidney damage. Overall, Ketorolac can be a useful tool in managing pain, but it's essential to follow proper guidelines and consult with a healthcare professional.
About
Health and Medicine
Latest Posts


Caffeine and Medication Safety: What You Need to Know About Dangerous Interactions
By Marcel Kornblum Jan 10, 2026
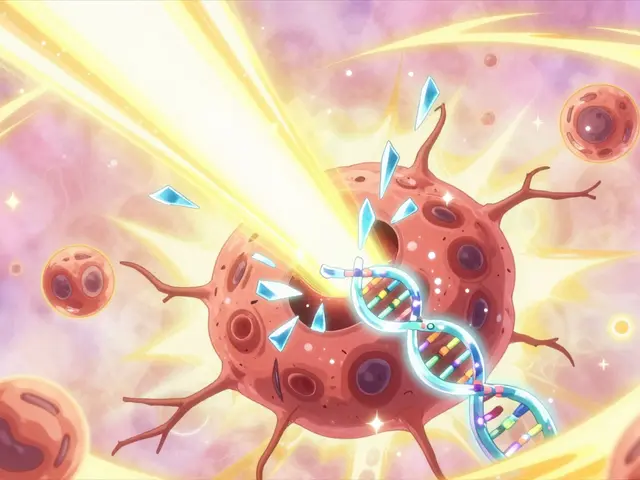
Radiation Therapy: How Radiation Destroys Cancer Cells at the DNA Level
By Marcel Kornblum Jan 5, 2026
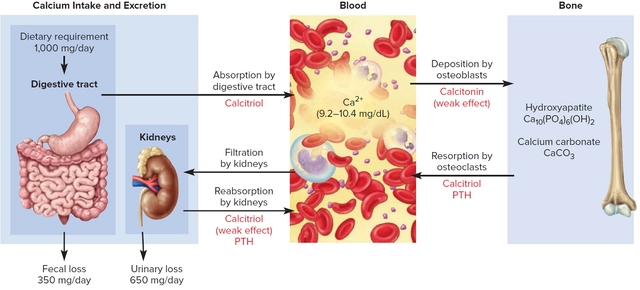
Understanding the side effects and risks of calcitonin therapy
By Marcel Kornblum May 29, 2023