Calcitonin Therapy: What It Is and Who It Helps
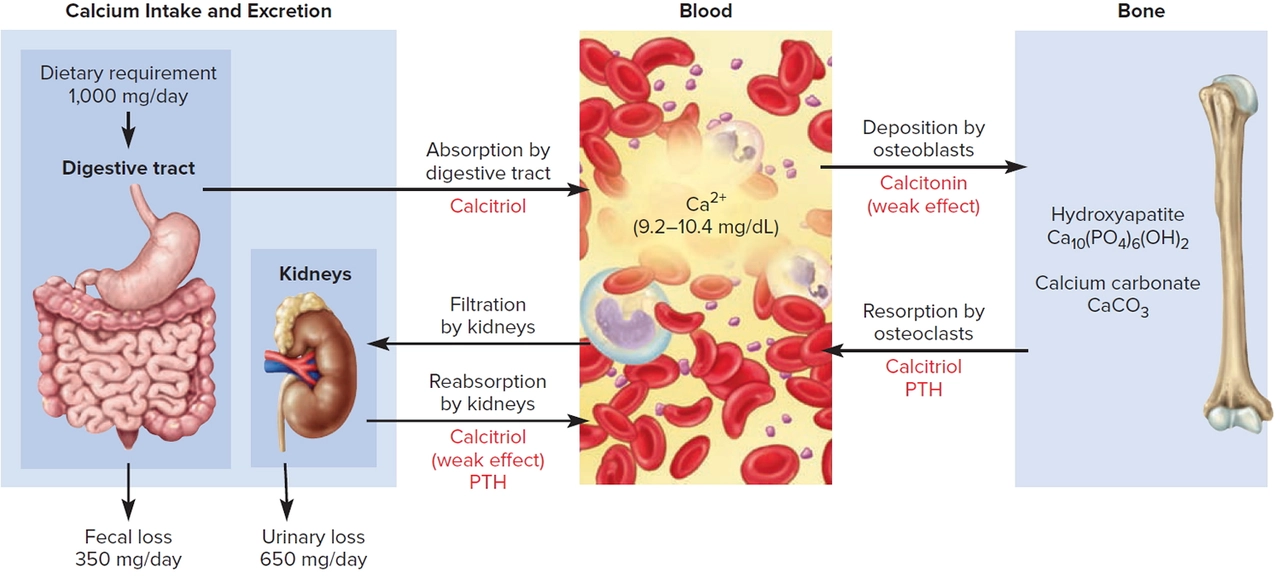
Calcitonin therapy uses a hormone (often salmon-derived) to lower blood calcium and help protect bone. You’ll see it most often for sudden high calcium levels, relief of bone pain, and as a second-line option for osteoporosis when other treatments aren’t suitable.
How it works is straightforward: calcitonin slows the cells that break down bone (osteoclasts). That reduces the amount of calcium released into the blood and can ease bone pain. Because many prescription forms come from salmon, the drug is usually called "salmon calcitonin."
When doctors pick calcitonin
Doctors usually use calcitonin in three situations. First, to treat acute hypercalcemia (dangerously high blood calcium) because it acts quickly to drop calcium levels. Second, for Paget’s disease of bone to reduce bone turnover and pain. Third, as a backup for osteoporosis when bisphosphonates or other first-line drugs aren’t an option or cause intolerable side effects.
Calcitonin is available as a nasal spray and as injections. The nasal spray is handy for longer symptom relief and is often used for bone pain or osteoporosis. Injections give a faster effect and are used in hospitals for severe hypercalcemia.
What to expect: dosing, side effects, and safety
Dosing varies by product. Nasal sprays are usually one spray in one nostril a day, and injections are given under a doctor’s guidance. Don’t try to adjust doses on your own—talk to your prescriber about the exact schedule for your condition.
Common side effects are mild: nasal irritation with the spray, flushing, nausea, or injection-site soreness. Some people report a salty or fishy taste. Serious allergic reactions are rare but possible, especially in people allergic to fish. If you notice swelling, rash, trouble breathing, or severe dizziness, seek emergency care.
Two practical points: the effect of calcitonin can wear off if used long term (tachyphylaxis), so doctors often limit continuous use. Also, its ability to prevent fractures is modest compared with newer osteoporosis drugs, so your provider may recommend alternatives first.
Monitoring is simple: expect follow-up blood tests for calcium and kidney function, and periodic bone density scans if you’re using it for osteoporosis. Tell your doctor about all medicines you take—there aren’t many strong drug interactions, but it’s smart to check.
Thinking about alternatives? For long-term bone protection, bisphosphonates, denosumab, or teriparatide are commonly preferred. For short-term control of high calcium, intravenous fluids and other meds may be combined with calcitonin.
If you’re considering calcitonin therapy, ask your clinician why it fits your situation, how long you’ll use it, and what to watch for at home. Small questions now can prevent surprises later.
Understanding the side effects and risks of calcitonin therapy
As a blogger, I've been researching calcitonin therapy and its potential side effects and risks. Calcitonin is a hormone used to treat conditions like osteoporosis and high levels of calcium in the blood. While this therapy can be beneficial, it's crucial to understand the possible side effects, which may include nausea, facial flushing, and skin reactions at the injection site. Rare but serious risks include low levels of calcium in the blood and an increased risk of certain types of cancer. It's essential to discuss these concerns with a healthcare professional before starting calcitonin therapy to ensure it's the right choice for your specific needs.
About
Health and Medicine
Latest Posts


Eurax (Crotamiton) vs Other Anti-Itch Medications: Pros, Cons & Alternatives
By Marcel Kornblum Oct 17, 2025

Arimidex (Anastrozole) vs Other Aromatase Inhibitors: A Practical Comparison
By Marcel Kornblum Oct 2, 2025

Actigall (Ursodiol) vs Alternatives: What Works Best for Gallstones and Liver Issues
By Marcel Kornblum Dec 1, 2025