Biologic drugs have changed how we treat cancer, autoimmune diseases, and chronic conditions. But they come with a price tag that can break the bank. A single year of treatment for a biologic like Humira or Enbrel can cost over $20,000 - sometimes more. For years, patients and insurers had no real alternative. Then came biosimilars. These aren’t generics. They’re not exact copies. But they’re close enough to work the same way - and save a lot of money.
What Exactly Is a Biosimilar?
A biosimilar is a biologic drug that’s highly similar to an already-approved biologic, called the reference product. It’s not a copy like a generic pill. Think of it this way: a generic aspirin is chemically identical to brand-name aspirin. A biosimilar is more like a handcrafted replica of a Rolex - same function, same precision, but made by a different factory with slightly different materials. The FDA requires biosimilars to show no clinically meaningful differences in safety, effectiveness, or purity. That means if your doctor prescribed Humira, a biosimilar version will work just as well for your rheumatoid arthritis or Crohn’s disease.
The first FDA-approved biosimilar hit the U.S. market in 2015. Since then, the number has grown slowly. By early 2025, there were 10 biosimilars approved for Humira alone. That’s a big deal - Humira was the top-selling drug in the world for years, bringing in over $20 billion annually. Now, those biosimilars are forcing prices down.
How Much Do Biosimilars Actually Save?
Here’s where it gets interesting. Biosimilars don’t slash prices by 80-90% like generics do. That’s because biologics are made from living cells - not chemicals. The manufacturing process is complex, expensive, and hard to replicate exactly. So the savings are more modest, but still huge.
On average, biosimilars cost 15% to 35% less than the original biologic when covered under medical benefits. But look at specific cases. In January 2025, when 10 Humira biosimilars entered the market, the list price dropped by as much as 85%. That’s not a discount - that’s a revolution. The same thing happened with Stelara (ustekinumab). Nine biosimilars launched in mid-2025, with prices up to 90% lower than the original list price.
But here’s the catch: list price isn’t what you pay. The U.S. drug pricing system is built on rebates, discounts, and hidden contracts between manufacturers, pharmacy benefit managers (PBMs), and insurers. So while the sticker price might be 85% lower, the actual net price - after rebates - might only be 30% lower. That’s why originator drugs still made up 98.9% of all biologic spending in 2023, even with biosimilars available.
Biosimilars vs. Generics: Why the Difference?
Generics are simple. They’re made from chemicals. The molecule is the same. The manufacturing is predictable. That’s why a generic version of Lipitor can cost 90% less than the brand.
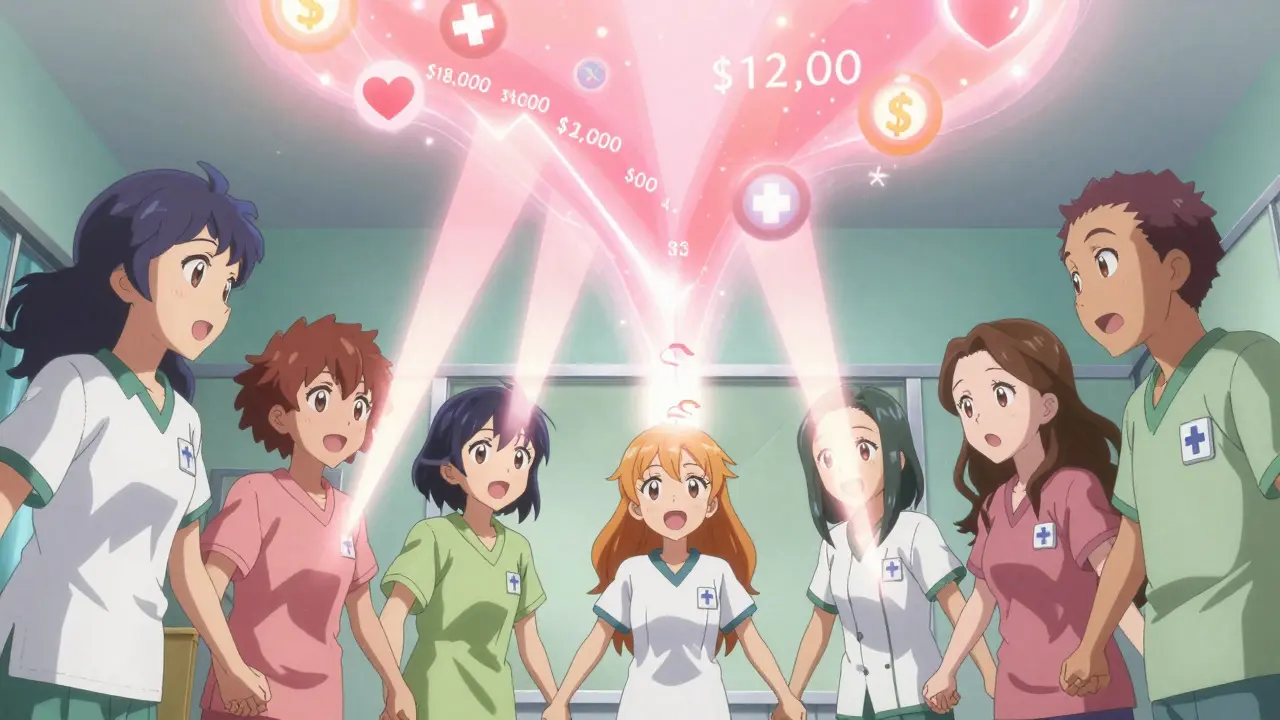
Biosimilars? They’re made in living cells - yeast, bacteria, or mammalian cells. Tiny changes in temperature, pH, or nutrient mix can alter the final product. That’s why they can’t be identical. The FDA requires more than 100 times the testing for a biosimilar than for a generic. That drives up development costs. So while a generic might cost $5 for a month’s supply, a biosimilar might cost $12,000 instead of $18,000. Still a massive win.
And unlike generics, biosimilars don’t automatically replace the original. Doctors don’t switch patients unless they’re confident in the safety and efficacy. That’s changing, though. A 2024 study in JAMA Network Open showed that biosimilar prices kept dropping after they entered the market - and more patients started using them over time.
Real-World Savings: Who’s Saving What?
The numbers aren’t just theoretical. In 2024 alone, biosimilars saved the U.S. healthcare system $20.2 billion. Since 2015, that total hits $56.2 billion. That’s money that didn’t go to drug companies - it went to patients, employers, and Medicare.
Employers are seeing direct benefits. One analysis found that if all employees switched from Humira to its biosimilar, an employer could save an average of $1.53 million per year. Across all self-insured U.S. companies, switching just two biologics to biosimilars could save $1.4 billion. For patients, out-of-pocket costs dropped by 23% on average when using biosimilars, according to CSRxP. For some, the savings were as high as 45%.
Medicare Part B has also seen price erosion. When biosimilars entered the market, the average payment for the biologic dropped by 20-30% within a year. That’s not just a discount - it’s a market correction.
The Big Problem: The Biosimilar Void
Here’s the scary part: we’re not even close to using all the potential savings. Over the next 10 years, 118 biologic drugs will lose patent protection. Only 12 of them have biosimilars in development. That means 90% of the upcoming biologics - drugs that could save billions - have no competition coming.
In Europe, 73% of high-selling biologics had biosimilars in the pipeline in 2023. In the U.S.? Only 23%. Why? Because developing a biosimilar is expensive - often $100 million to $200 million - and the U.S. market is hard to crack. Rebates, formulary restrictions, and fear of switching make it risky for manufacturers.
That’s a $234 billion opportunity lost. If we had the same biosimilar adoption rate as Norway - where 86% of patients use biosimilars for certain biologics - we’d be saving tens of billions more each year.

How to Get the Most Out of Biosimilars
If you’re a patient, ask your doctor: Is there a biosimilar for my drug? It’s safe. It’s effective. And it’s cheaper.
If you’re an employer or insurer, here’s what works:
- Put biosimilars on the preferred tier in your formulary
- Require step therapy - try the biosimilar before approving the original
- Negotiate contracts that reward biosimilar use, not rebates on expensive brands
- Use data tools like Segal’s SHAPE warehouse to track spending and utilization
Don’t fall for the rebate trap. A drug with a $20,000 list price and a 50% rebate might look cheaper than a $12,000 biosimilar with no rebate - but you’re paying for complexity, not savings. Look at net cost, not list price.
The Future Is Here - But It’s Not Moving Fast Enough
Biosimilars aren’t the future. They’re the present. They’ve been saving lives and money for a decade. But the system is still stuck in old patterns. PBMs favor rebates. Doctors hesitate to switch. Patients don’t know the difference.
The FDA is making it easier to approve biosimilars. The Inflation Reduction Act is pushing Medicare to favor lower-cost options. The Biden administration has targeted drug pricing reform. But real change needs more than policy - it needs action.
Every biosimilar that enters the market brings down prices for everyone - even the original drug. When a second biosimilar enters within three years of the first, prices drop even faster. That’s competition. That’s what markets are supposed to do.
Right now, we’re letting billions slip away. We have the science. We have the approvals. We have the evidence. What we’re missing is the will to use it.
It’s not about choosing between safety and savings. It’s about choosing both. Biosimilars deliver. The question is - who’s going to make sure we all get to use them?






Kenji Gaerlan
January 23, 2026 at 07:48
biosimilars are cool and all but why do we even need them when big pharma just raises prices anyway? like who even cares if it’s 15% cheaper when the list price is still 20k?