Acetaminophen Overdose Risk Calculator
How much acetaminophen are you taking?
Check if your daily intake exceeds safe limits and get immediate guidance on liver protection.
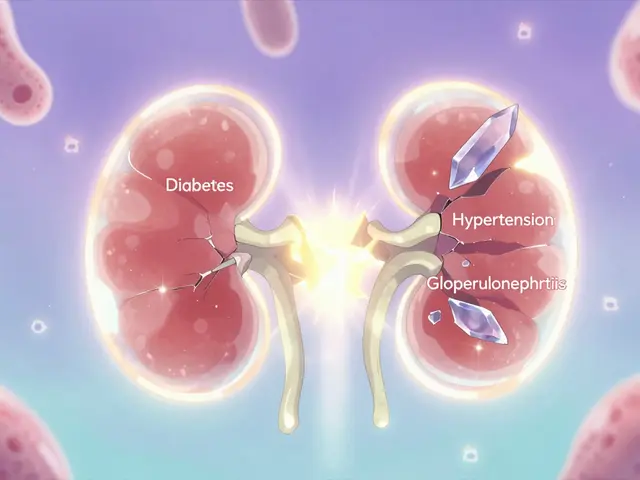
Most people assume that if a drug is prescribed or sold over the counter, it’s safe. But what if your medicine is quietly damaging your liver - without you knowing until it’s too late? Medication-related liver damage, or drug-induced liver injury (DILI), is more common than you think. It’s not rare. It’s not exotic. And it doesn’t only happen with illegal drugs or massive overdoses. It can start with a simple antibiotic, a popular herbal supplement, or even your daily pain reliever. The scary part? You might not feel anything until your liver is already failing.
How Common Is Medication-Related Liver Damage?
About 1 in 5,000 people taking a new medication will develop some form of liver injury. That’s not a tiny number. In Western countries, DILI causes around 13 to 19 cases per 100,000 people every year. It’s now the leading cause of acute liver failure in the U.S., surpassing viral hepatitis. And it’s rising. Between 2015 and 2022, cases increased by 27% in Europe - mostly because of herbal and dietary supplements that aren’t properly tested for safety.
Antibiotics like amoxicillin-clavulanate are the biggest culprits, responsible for nearly 1 in 6 cases. But don’t assume prescription drugs are the only problem. Herbal products - things like green tea extract, kava, and turmeric - cause 20% of DILI cases in the UK and are climbing fast in the U.S. Many people think “natural” means safe. It doesn’t. Green tea extract alone is linked to 37% of all supplement-related liver injuries.
What Does Liver Damage from Medication Actually Feel Like?
The problem with DILI is that it doesn’t always scream for attention. Early signs are easy to ignore. You feel tired. Your appetite drops. Maybe you have a dull ache under your right ribs. You chalk it up to stress, the flu, or just getting older. But these are the first whispers of trouble.
When the liver starts failing, clearer signs show up:
- Yellow skin or eyes (jaundice) - This is the red flag. It means bilirubin is building up because your liver can’t process it.
- Dark urine - Like tea or cola. That’s not normal. It’s a sign your liver is leaking bile into your bloodstream.
- Light-colored stools - Pale, clay-colored poop? That’s bile not reaching your intestines.
- Severe itching - Not just a rash. A deep, unrelenting itch, especially at night. This is caused by bile salts building up in your skin.
- Nausea, vomiting, or abdominal pain - Especially under your right rib cage. That’s where your liver sits.
If you have jaundice and any two of these other symptoms - dark urine, right-side pain, nausea - within eight weeks of starting a new medication, you need to go to the emergency room now. Waiting another day could cost you your life.
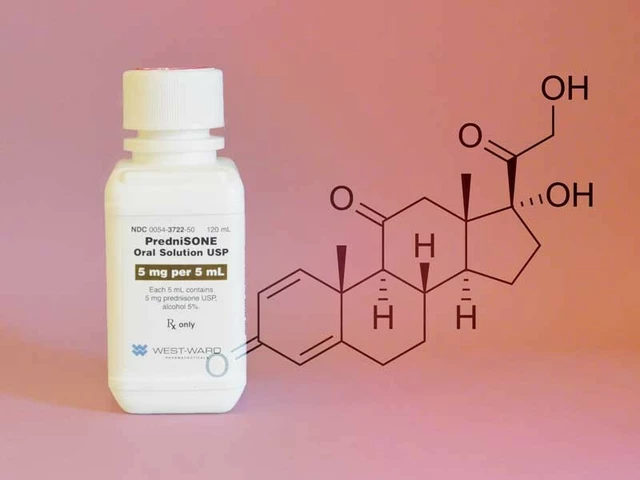
Acetaminophen: The Silent Killer in Your Medicine Cabinet
Acetaminophen - Tylenol, Paracetamol - is the most common cause of acute liver failure in the U.S. and Australia. But it’s not just overdoses. People take it for days, thinking they’re being careful. The FDA says healthy adults shouldn’t exceed 3,000 mg per day. That’s six 500 mg pills. Many don’t realize that cold medicines, pain relievers, and sleep aids often contain acetaminophen too. Stack them up, and you’re over the limit without even knowing.
And if you drink alcohol? Your risk triples to five times higher. Even one drink a day while taking acetaminophen can push you into danger. The damage happens fast. Liver enzymes spike within 24 hours of overdose. By 72 hours, your liver may be in free fall. Treatment with N-acetylcysteine works best if given within 8 hours. After that, effectiveness drops by 10% every hour. By 24 hours, it’s often too late.

Why Doctors Miss It - And How to Protect Yourself
Studies show that 68% of DILI patients were initially misdiagnosed. Doctors thought it was the flu, gallstones, or stress. Patients didn’t connect their symptoms to medication because they didn’t know to look. One patient on Healthgrades said: “I had itching for two weeks on amoxicillin-clavulanate. My doctor said it was an allergic reaction. It wasn’t. My liver enzymes were 15 times normal.”
There’s no single blood test that confirms DILI. Diagnosis relies on ruling everything else out - viral hepatitis, gallstones, autoimmune disease. The RUCAM scoring system is used by specialists to link drug exposure to liver injury, but most GPs don’t use it. That’s why you need to be your own advocate.
Here’s what you can do:
- Keep a full medication log - Write down every pill, capsule, tea, or powder you take. Include brand names, doses, and start dates. Include supplements. Even if your naturopath says they’re “safe.”
- Ask your doctor - “Is this drug known to affect the liver?” Don’t assume they know. Only 42% of primary care doctors correctly identify high-risk medications in surveys.
- Check for warning labels - The FDA now requires black box warnings on many antibiotics for liver risk. Look for them.
- Don’t ignore itching - It’s the most underreported symptom. If you’re itchy and on a new drug, get your liver checked.
Supplements Are Not Regulated - And That’s Dangerous
Green tea extract, kava, pyrrolizidine alkaloid-containing herbs (like comfrey), and even “liver cleanse” blends have caused liver failure and transplants. The British Liver Trust says 20% of DILI cases come from supplements. The FDA doesn’t test them before they hit shelves. Manufacturers don’t have to prove safety - only that they don’t contain illegal substances.
One Reddit user wrote: “My naturopath told me my liver enzymes were high because I was ‘detoxing.’ That’s not a thing. My liver was failing.”
There’s no such thing as a “detox” that needs to damage your liver. If your liver enzymes are sky-high after taking a supplement, stop it immediately - and get tested. No amount of “natural healing” can fix a liver that’s shutting down.

When to Act - The Exact Moments You Can’t Afford to Wait
You don’t need to wait for a doctor’s appointment if you see these signs:
- Jaundice + dark urine + nausea - Go to the ER. Now.
- Acetaminophen overdose - Even if you feel fine. Call poison control or go to the hospital within 8 hours.
- Itching for more than a week - Especially if you’re on antibiotics or a supplement.
- Unexplained fatigue and loss of appetite - Lasting longer than 10 days after starting a new drug.
For people on long-term high-risk drugs like isoniazid (used for tuberculosis), weekly liver enzyme tests are recommended. Ten percent of users develop abnormal enzymes within three months. Catching it early means stopping the drug before permanent damage.
What Happens After Diagnosis?
Most cases of DILI get better if you stop the drug early. Your liver is an amazing organ - it can regenerate. But if you keep taking the medicine, you risk chronic injury, cirrhosis, or the need for a transplant. In severe cases, patients end up on the transplant list because they ignored early symptoms.
There’s no cure for DILI other than stopping the drug. No supplements, no teas, no “liver support” formulas will reverse it. The only thing that works is removing the cause and letting your body heal.
Some new tools are emerging. The FDA approved DILI-Alert, a smartphone app that checks your meds against a database of 1,200 liver-toxic substances. It’s not perfect, but it’s a step forward. AI systems are also cutting diagnosis time by 35% in pilot programs - meaning fewer people will wait months to get help.
Bottom Line: Your Liver Can’t Talk. You Have to Listen.
Medication-related liver damage doesn’t come with a warning siren. It whispers. It hides behind fatigue. It masquerades as a cold. It’s silent until it’s too late. The good news? Most cases are preventable. You don’t need to avoid all medicine. You just need to know the risks, track what you take, and act fast when something feels wrong.
If you’re on a new medication and feel off - don’t wait. Don’t assume it’s nothing. Get your liver checked. It could save your life.
Can over-the-counter painkillers damage my liver?
Yes. Acetaminophen (Tylenol, Paracetamol) is the most common cause of drug-induced liver failure in the U.S. and Australia. Taking more than 3,000 mg per day - even spread out over several days - can cause serious harm. Many cold and flu medicines also contain acetaminophen, so it’s easy to accidentally overdose. Never take more than one product with acetaminophen at a time, and avoid alcohol when using it.
Are herbal supplements safe for my liver?
No, not necessarily. Herbal and dietary supplements are not regulated like prescription drugs. Green tea extract, kava, and turmeric have all caused severe liver injury - including cases requiring transplants. A 2022 British Liver Trust report found green tea extract caused 37% of supplement-related liver damage. Just because something is “natural” doesn’t mean it’s safe for your liver.
What are the first signs of liver damage from medication?
Early signs are subtle: fatigue, loss of appetite, mild nausea, or a dull ache under your right ribs. But the first clear warning signs are yellow skin or eyes (jaundice), dark urine, light-colored stools, and severe itching - especially if they appear within 8 weeks of starting a new medication. If you have jaundice plus any two of those other symptoms, seek emergency care immediately.
How long does it take for medication to damage the liver?
It varies. Antibiotics like amoxicillin-clavulanate usually cause injury within 1 to 8 weeks, with an average of 15 days. Anticonvulsants take longer - around 45 days on average. Herbal supplements can cause damage anytime from 1 day to a year after starting. Acetaminophen overdose shows signs within 24 hours. If you’re on a new drug and feel unwell after a few days or weeks, consider liver damage as a possibility.
Should I get my liver tested if I’m on long-term medication?
If you’re on high-risk medications like isoniazid, methotrexate, or certain anticonvulsants, yes. Your doctor should monitor your liver enzymes regularly - often every 4 to 8 weeks. Even if you feel fine, abnormal enzymes can appear before symptoms. For most people on common drugs, routine testing isn’t needed unless symptoms arise. But if you’re taking multiple medications or supplements, ask your doctor about baseline liver tests.
Can I recover from medication-induced liver damage?
Yes - if you catch it early. Stopping the offending drug is the only treatment needed in most cases. The liver has a strong ability to regenerate. Many people return to normal liver function within weeks or months. But if damage continues because the drug isn’t stopped, it can lead to chronic liver disease, cirrhosis, or liver failure. Never ignore symptoms like jaundice or severe itching - they’re your body’s last warning.



Karen Mccullouch
December 14, 2025 at 05:04
I can't believe people still trust Big Pharma! My cousin took Tylenol for a headache and ended up in the ICU. They didn't even tell her it could kill her liver. 🤬