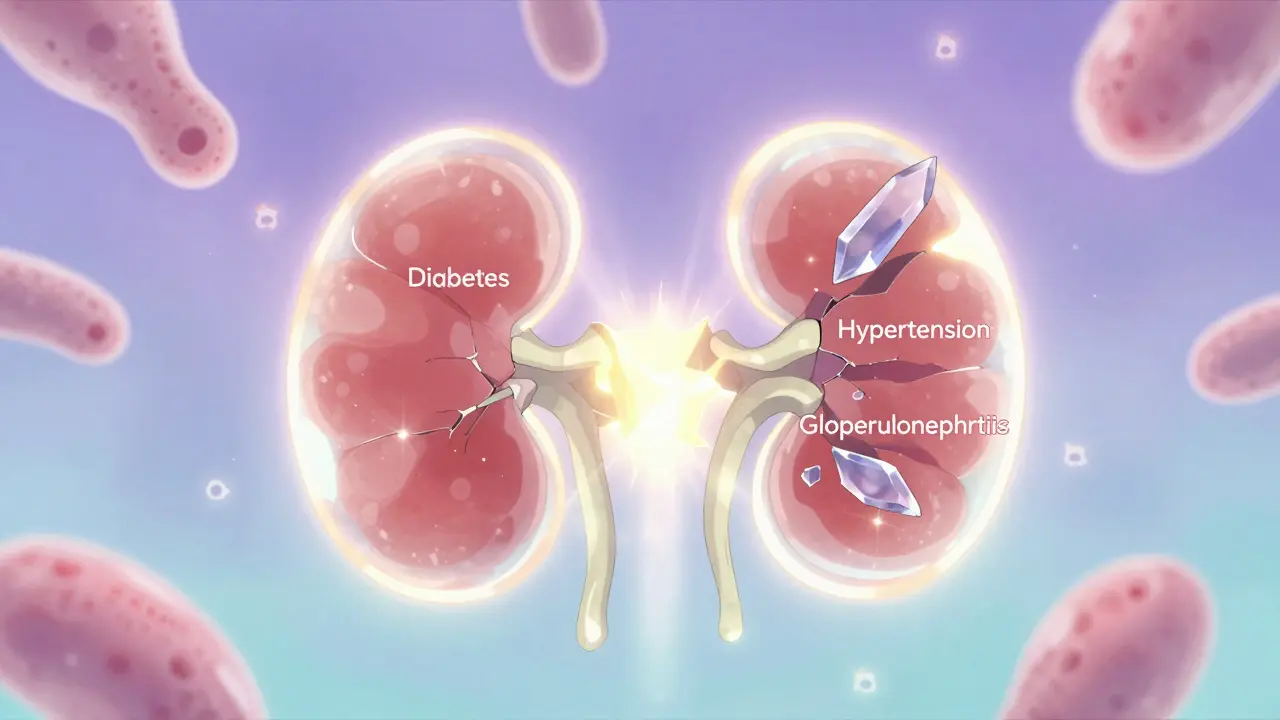
When your kidneys stop working, it’s not a sudden event. It’s a slow leak-years of damage building up before you even notice something’s wrong. By the time symptoms show up, up to 90% of kidney function may already be gone. The three biggest reasons this happens? Diabetes, hypertension, and glomerulonephritis. Together, they cause nearly 80% of all kidney failure cases in the U.S. and most high-income countries. But knowing how each one works makes all the difference in stopping it before it’s too late.
Diabetes: The Silent Kidney Killer
Diabetes doesn’t just affect your blood sugar-it rewires your kidneys. High glucose levels force your kidneys to filter too much blood. That sounds good, right? But over time, that extra work damages the tiny filters inside your kidneys, called glomeruli. The first sign? Protein starts leaking into your urine. That’s not normal. Healthy kidneys hold onto protein. When it shows up in urine tests, it’s a red flag.
By the time someone with type 2 diabetes gets diagnosed, many have already had undetected kidney damage for years. About 40% of people with type 2 diabetes develop diabetic kidney disease. For type 1, it’s about 30%. The damage builds slowly: the basement membrane of the glomeruli thickens from 300-400 nanometers to over 600 nm. Tiny cells called podocytes start dying. Blood vessels in the kidney harden. The result? Your kidneys can’t clean your blood anymore.
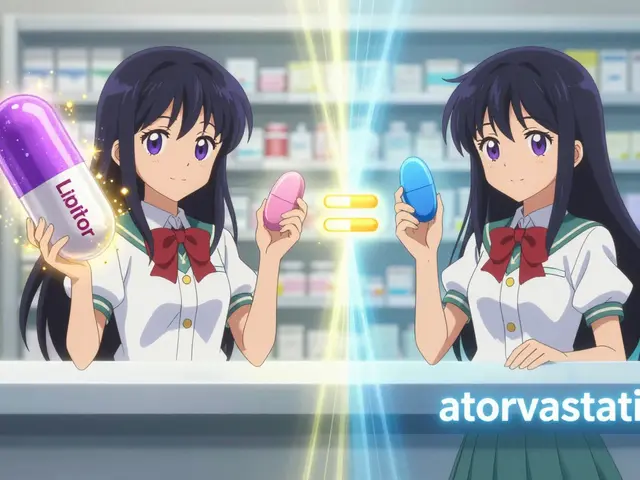
The good news? Early action works. If you get your HbA1c below 7% within the first five years of diagnosis, you cut your risk of kidney failure by more than half. Medications like SGLT2 inhibitors (dapagliflozin, empagliflozin) don’t just lower blood sugar-they protect your kidneys directly. In the EMPA-KIDNEY trial, these drugs reduced the risk of kidney failure by 32%. They’re now recommended as soon as urine protein levels rise above 30 mg/g, even if your kidney function looks normal.
Hypertension: The Pressure That Crushes Kidneys
High blood pressure doesn’t just strain your heart-it crushes your kidneys. When your blood pressure stays above 140/90 mmHg, the small arteries feeding your kidneys start to thicken and harden. This is called nephrosclerosis. Less blood reaches the filtering units. Without enough blood flow, the glomeruli shrink and scar. Studies show that 60-70% of people with long-term uncontrolled hypertension have scarring in 25-40% of their glomeruli.
What makes hypertension especially dangerous is how often it teams up with diabetes. Three out of four people with diabetes also have high blood pressure. Together, they speed up kidney damage by more than 75%. While diabetes alone causes kidney function to drop about 1.8 mL/min per year, the combo drops it by 3.2 mL/min. That’s a huge difference over five or ten years.
Controlling blood pressure is non-negotiable. The target for people with kidney disease is now <130/80 mmHg. For those with protein in their urine, it’s even lower-<120/80 mmHg. ACE inhibitors and ARBs are the go-to drugs because they don’t just lower pressure-they reduce protein leakage and slow scarring. But here’s the catch: many people don’t feel high blood pressure. No headaches. No dizziness. That’s why it’s called the silent killer. If you’re not getting checked regularly, you’re flying blind.
Glomerulonephritis: When Your Immune System Attacks Your Kidneys
Unlike diabetes and hypertension, glomerulonephritis isn’t about wear and tear. It’s an attack. Your immune system, meant to protect you, turns on your kidneys. It’s not one disease-it’s a group of disorders, each with different triggers. The most common form globally? IgA nephropathy. It’s where immune complexes build up in the glomeruli, causing inflammation. In Western countries, it affects 2.5 people per 100,000 each year. In parts of Asia, that number jumps to 4.5 per 100,000.
Another major type is lupus nephritis, which happens in half of people with systemic lupus. Depending on the pattern of damage seen in a kidney biopsy, 10-30% of these patients will end up needing dialysis within 10 years. The worst cases-classified as class IV-have a 28.7% chance of kidney failure.
Here’s the hard truth: glomerulonephritis often flies under the radar. People ignore swelling in their ankles, foamy urine, or dark-colored urine. One patient on Reddit said he saw seven doctors over 18 months before getting diagnosed. By then, his kidneys were already failing. Biopsies show IgA deposits under the microscope, but by the time you see them, damage may be advanced.
Treatment is different too. You can’t just control blood sugar or pressure. You need to calm the immune system. Drugs like rituximab have been shown to cut ESRD risk by nearly half in high-risk IgA patients. But it’s not for everyone. Some experts warn that aggressive immunosuppression in older patients raises infection risk without clear kidney benefit. It’s a tight balance-treating early enough to save the kidneys, but not so hard that you put the patient at new risk.

How Fast Do They Progress? The Numbers Don’t Lie
Not all kidney failure happens at the same speed. Diabetic kidney disease tends to move faster. From the first sign of protein in urine to needing dialysis? About 8.7 years on average. Hypertensive kidney disease takes longer-12.3 years. But glomerulonephritis? It’s a wild card. Some people stay stable for decades. Others crash in five years.
For diabetics, the risk jumps dramatically with urine protein levels:
- Normal protein (<30 mg/g): 1% risk of ESRD in 5 years
- Microalbuminuria (30-300 mg/g): 8% risk
- Macroalbuminuria (>300 mg/g): 44% risk
That’s why testing matters. If you have diabetes or high blood pressure, you need a urine albumin-to-creatinine ratio (UACR) test every year-or every three months if protein is already present. Blood tests for eGFR are just as important. You can’t rely on how you feel. By the time you’re tired, swollen, or nauseous, it’s often too late for simple fixes.
What Works? The Science Behind Real Protection
There’s no magic pill, but there are proven strategies:
- SGLT2 inhibitors for diabetics: Reduce kidney failure risk by 32%, heart failure by 30%. Now first-line for anyone with albuminuria.
- ACE inhibitors or ARBs: Cut protein leakage by 20-30% across all causes. Essential for anyone with kidney disease and high blood pressure.
- Finerenone: A newer drug approved in 2023 that blocks a hormone linked to kidney scarring. Reduces kidney failure risk by 18% in diabetics with proteinuria.
- Sparsentan: Coming soon, this dual-action drug cut proteinuria by nearly 50% in glomerulonephritis patients in 2023 trials.
But drugs alone aren’t enough. Diet matters. Too much salt raises blood pressure. Too much protein overworks damaged kidneys. The recommended intake is 0.8 grams per kilogram of body weight. Most people don’t hit that mark. In fact, 63% of kidney patients struggle to stick to it.
And adherence? It’s terrible. Only 58% of people take their blood pressure meds consistently after a year. That’s why follow-up care is critical. You need a team-nephrologist, dietitian, primary care doctor-to keep you on track.
Why Early Detection Is Everything
The biggest mistake? Waiting for symptoms. Fatigue, swelling, nausea-those are late signs. By then, your kidneys are already failing. The real window for saving them is before you feel anything. That’s why regular screening is the most powerful tool you have.
If you have diabetes, get your urine tested every year. If you have high blood pressure, do the same. If you notice foamy urine, puffiness around your eyes, or unexplained swelling in your legs, don’t wait. Ask for a UACR test and an eGFR blood test. These cost less than $50 in most places and take less than five minutes.
One patient in a National Kidney Foundation survey said she stabilized her kidney function after starting an SGLT2 inhibitor just six months after her first protein leak. She didn’t wait. She acted. That’s the difference between needing dialysis and living well.
Global data shows we could prevent 30-50% of future kidney failures if everyone with diabetes or hypertension got screened and treated early. It’s not about expensive treatments. It’s about catching it before it’s too late.
What Comes Next?
Research is moving fast. New biomarkers like urinary TNF receptor-1 can predict kidney failure five years ahead with 89% accuracy. That’s a game-changer. Instead of waiting for protein to show up, we’ll be able to spot trouble before it starts.
But technology won’t help if people don’t get tested. In low-income countries, only 10% of people with kidney failure get dialysis. In the U.S., it’s 95%. That’s not just a medical gap-it’s a justice gap.
If you’re at risk-because of diabetes, high blood pressure, or family history-don’t wait. Talk to your doctor. Get tested. Start early. Your kidneys don’t scream. They whisper. And if you don’t listen, they’ll go silent.
Can you reverse kidney damage from diabetes?
Early-stage kidney damage from diabetes can be slowed or even partially reversed with strict blood sugar control, blood pressure management, and medications like SGLT2 inhibitors. Once scarring and significant loss of filtering units occur, it’s permanent. The goal isn’t reversal-it’s stopping further damage. The earlier you act, the better your chances.
Is high blood pressure always bad for kidneys?
Not always-but uncontrolled high blood pressure is. Blood pressure below 130/80 mmHg is protective. But if it stays above 140/90 for years, it damages the small arteries in the kidneys, leading to scarring and reduced blood flow. The risk increases the longer it’s untreated. Even if you feel fine, high blood pressure is quietly harming your kidneys.
What are the early signs of glomerulonephritis?
Early signs are often subtle: foamy urine (from protein), dark or cola-colored urine (from blood), swelling in ankles or face, and high blood pressure. Many people have no symptoms at all until damage is advanced. A simple urine test can detect protein or blood before you feel anything. Don’t wait for symptoms-get tested if you’re at risk.
Do I need a kidney biopsy to diagnose glomerulonephritis?
Not always, but often. Blood and urine tests can suggest it, but a biopsy is the only way to confirm the exact type of glomerulonephritis and see how much damage has occurred. That’s critical because treatment depends on the subtype. For example, IgA nephropathy and lupus nephritis need very different drugs. If your doctor suspects immune-related kidney disease, a biopsy is usually recommended.
Can lifestyle changes alone prevent kidney failure?
Lifestyle changes-low salt, healthy weight, no smoking, regular exercise-are essential. But for most people with diabetes or hypertension, they’re not enough on their own. Medications like ACE inhibitors, ARBs, and SGLT2 inhibitors have been proven to reduce kidney failure risk by 20-50%. Lifestyle supports the meds-it doesn’t replace them. The most effective plan combines both.
How often should I get my kidneys checked if I have diabetes?
At least once a year. If you already have protein in your urine (microalbuminuria), get tested every 3-6 months. Your doctor should check your urine albumin-to-creatinine ratio (UACR) and your eGFR (blood test) annually. More frequent checks are needed if your numbers are changing or if you’re starting a new kidney-protective medication.
Next steps: If you have diabetes or high blood pressure, ask your doctor for your latest UACR and eGFR results today. If you don’t know what they mean, ask for an explanation. Write them down. Set a reminder to check them again in six months. Kidney failure doesn’t happen overnight-but it can be stopped, if you act before it’s too late.


Ian Long
January 7, 2026 at 19:46
Man, I’ve seen this play out with my uncle. Diabetic for 15 years, never checked his urine until he started swelling up. By then? He was on dialysis. They didn’t even tell him protein in urine was a red flag until it was too late. SGLT2 inhibitors? His doc waited too long. Don’t wait. Test early.