Cumulative Drug Toxicity Calculator
Drug Safety Calculator
Track your cumulative drug exposure to see if you're approaching potentially dangerous levels. Many drugs accumulate in the body over time, increasing toxicity risk even at normal doses.
Think your medication is safe because you’ve been taking it for years without problems? That’s a dangerous assumption. Many drugs don’t hurt you right away-they quietly build up in your body, inching closer to a breaking point. This is cumulative drug toxicity: side effects that sneak up after months or even years of use, often when you least expect them.
How Drugs Accumulate in Your Body
Your body is designed to process and get rid of drugs. But not all drugs are created equal. Some are cleared quickly. Others? They stick around. When you take a drug faster than your body can eliminate it, the leftovers pile up. That’s accumulation. And over time, that pile becomes a problem.Drugs with long half-lives are the biggest culprits. A half-life is how long it takes for half the drug to leave your system. If a drug’s half-life is over 24 hours, it’s already on track to build up. Some, like amiodarone (used for irregular heart rhythms), can hang around for months. One patient developed lung scarring after taking just 600 grams total-over several years. Their blood levels looked fine at every checkup. But the drug wasn’t in their blood. It was in their lungs.
Fat-soluble drugs are especially sneaky. Vitamins A, D, E, and K don’t dissolve in water. They store in your fat tissue and bone. Heavy metals like lead and mercury do the same. Once they’re in, they’re hard to get out. Elimination can take 50 to 200 days. That’s why people on long-term antibiotics, heart meds, or cancer drugs often don’t feel sick until it’s too late.
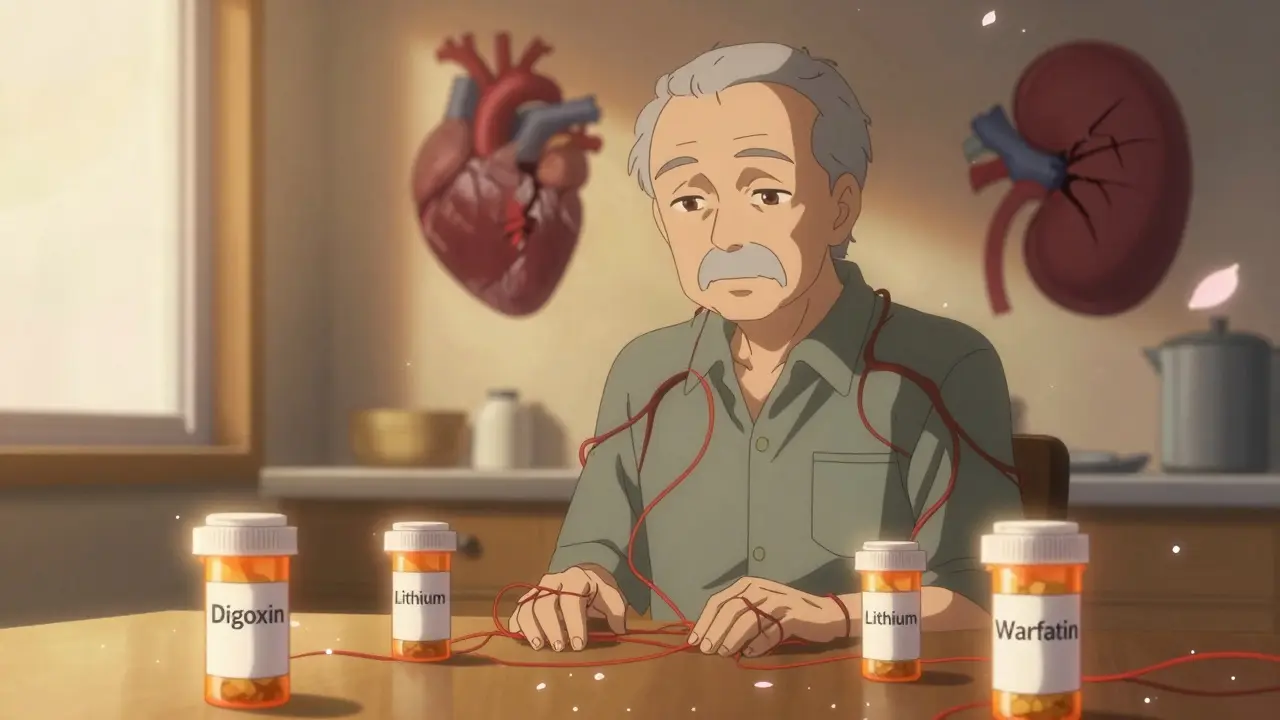
Why Older Adults Are at Higher Risk
As you age, your liver and kidneys slow down. They don’t filter drugs as well. Studies show that in older adults, drug metabolism can drop by 30% to 50%. That means a dose that was safe at 50 might become toxic at 70.The American Geriatrics Society Beers Criteria lists 34 medications with high risk for cumulative toxicity in seniors. One example: digoxin, a heart medication. Even small increases in blood levels can cause nausea, confusion, or dangerous heart rhythms. Many patients don’t realize their symptoms are drug-related. They blame aging, stress, or diet.
And here’s the kicker: 68% of adverse drug reactions in elderly patients are due to cumulative effects, not sudden overdoses. That’s not rare. That’s common. Yet most doctors don’t track total lifetime doses. They check blood levels once a month and assume everything’s fine. But if the drug is stored in fat, your blood level doesn’t tell the whole story.
Cancer Drugs and the Hidden Cost of Treatment
Cancer patients are among the most studied when it comes to cumulative toxicity. Why? Because they get high-dose drugs for months, sometimes years.Take anthracyclines, a class of chemo drugs. The lifetime maximum dose is 450 mg/m². Exceed that, and your risk of permanent heart damage jumps sharply. That limit wasn’t pulled from thin air. It came from 17 clinical trials with over 8,500 patients. Yet, in real life, many patients get more than that-especially if they switch treatments or get re-treated after a relapse.
A 2019 study in the Journal of the National Cancer Institute tracked toxicity in patients on targeted cancer drugs. In the first treatment cycle, about 25% had side effects. By the sixth cycle, that number dropped to 2%. Sounds good, right? But here’s the truth: the total number of patients who experienced serious toxicity by cycle six was over 50%. The side effects didn’t disappear-they just spread out. One person got tired. Another had nerve pain. A third developed liver issues. Individually, each symptom seemed minor. Together, they added up to a life-altering condition.
What Medications Are Most Likely to Build Up?
Not all drugs are risky. But some are known for cumulative effects. Here are the big ones:- Amiodarone - Heart rhythm drug. Can cause lung, liver, and thyroid damage after months of use.
- Digoxin - Heart failure drug. Narrow safety window. Toxicity builds slowly, often mistaken for dementia.
- Lithium - Mood stabilizer. Kidney and thyroid damage can occur after years. Blood tests don’t always catch it.
- Aminoglycosides - Antibiotics like gentamicin. Can cause permanent hearing loss or kidney damage with repeated use.
- Methotrexate - Used for rheumatoid arthritis and some cancers. Liver and bone marrow toxicity accumulates over time.
- Warfarin and other anticoagulants - Bleeding risk increases with long-term use, especially if kidney function declines.
These aren’t rare drugs. Millions of people take them. And most patients have no idea their doctor should be tracking total lifetime exposure.
Why Monitoring Often Fails
You’d think doctors would track total doses. But they rarely do. Why?First, most electronic health records don’t calculate cumulative doses automatically. A doctor sees a patient, writes a prescription, and moves on. They don’t have a running total of how much amiodarone you’ve taken since 2018.
Second, many patients don’t keep track. They switch pharmacies. They get prescriptions from different doctors. One doctor prescribes warfarin. Another prescribes a new antibiotic. Neither knows what the other prescribed.
Third, blood tests lie. For fat-soluble drugs, your blood level might be normal while your organs are saturated. A 2022 Medscape survey found that 82% of doctors blamed patient non-adherence for missed toxicity. But the real issue? We’re not measuring the right thing.
There’s a case from Reddit’s r/medicine: an oncologist shared that a patient on long-term amiodarone developed pulmonary fibrosis. Her blood levels were always in range. Her liver tests were fine. But the drug had been building up in her lungs for five years. By the time she got breathless, it was too late.

What Can You Do?
You can’t stop taking necessary meds. But you can protect yourself.- Ask your doctor: “What’s the maximum lifetime dose for this drug? Am I close?”
- Keep your own log: Write down every prescription, the dose, and when you started. Use a notebook or phone app. Don’t rely on pharmacies or doctors to remember.
- Know your symptoms: Fatigue, nausea, tingling, memory fog, shortness of breath, or unusual bruising after years on a drug? That’s not normal aging. Ask if it could be drug-related.
- Get baseline tests: If you’re on a high-risk drug, ask for liver, kidney, thyroid, and heart function tests before you start. Repeat them yearly.
- Ask about alternatives: Is there a drug with less accumulation risk? For example, some newer anticoagulants don’t build up like warfarin.
Pharmacists can help too. A 2023 report from the American Pharmacists Association found that pharmacist-led monitoring cut hospital admissions for drug toxicity by 29%. Talk to your pharmacist. They’re trained to spot these patterns.
The Bigger Picture: What’s Changing
The system is slowly waking up. The FDA now requires cumulative toxicity warnings on 78% of new cancer drugs-up from 52% in 2017. The European Medicines Agency made cumulative assessments mandatory for all chronic-use drugs in January 2024. That’s huge.Some hospitals are using AI to predict individual risk. Memorial Sloan Kettering is testing models that analyze 27 factors-age, weight, genetics, kidney function-to forecast who’s likely to hit toxicity. Early results show 82% accuracy.
But here’s the gap: only 38% of U.S. electronic health records can auto-calculate cumulative doses. Most doctors are still flying blind.
Final Thought: Your Body Keeps Score
Medicines are powerful. They save lives. But they’re not harmless. Just because you feel fine doesn’t mean your body is fine. Toxicity doesn’t announce itself with a siren. It whispers-through fatigue, memory lapses, a dry cough, or a slow heartbeat. By the time it shouts, the damage may be permanent.If you’ve been on the same meds for years, don’t assume safety. Ask questions. Track your doses. Know your limits. Your future self will thank you.
Can cumulative drug toxicity be reversed?
Sometimes, yes-if caught early. Stopping the drug can stop further buildup, and your body may slowly clear the excess. But damage to organs like the liver, kidneys, lungs, or nerves can be permanent. The earlier you stop, the better your chances of recovery. That’s why tracking matters.
Do over-the-counter drugs cause cumulative toxicity?
Yes. Long-term use of NSAIDs like ibuprofen or naproxen can cause kidney damage or stomach bleeding that builds up slowly. Acetaminophen (Tylenol) can cause liver damage if taken daily for months, even at recommended doses. Herbal supplements like kava or comfrey can also accumulate and harm the liver. Just because it’s sold without a prescription doesn’t mean it’s safe for long-term use.
Why don’t doctors monitor cumulative doses more often?
Most electronic health records don’t track total lifetime doses. Doctors are busy, and there’s no standard system to alert them when a patient is approaching dangerous levels. It’s not negligence-it’s a system flaw. Patients need to take the lead in tracking their own exposure.
Is cumulative toxicity only a problem for older people?
No. While older adults are more vulnerable due to slower metabolism, younger people with liver or kidney disease, genetic differences in drug-processing enzymes, or those taking multiple medications are also at risk. Even healthy 30-year-olds on long-term antibiotics or antidepressants can develop cumulative effects.
How long does it take for cumulative toxicity to develop?
It varies. For some drugs, like lithium or amiodarone, it can take 6 months to 2 years. For others, like certain antibiotics or chemo drugs, it may take just a few cycles. There’s no universal timeline. It depends on the drug, your body, your health, and your dose.
Can genetic testing help predict cumulative toxicity risk?
Yes, in some cases. Genetic tests can show if you’re a slow or fast metabolizer of certain drugs. For example, people with a CYP2D6 poor metabolizer variant process codeine and some antidepressants very slowly, increasing risk of buildup. While not routine yet, this testing is becoming more common in oncology and psychiatry.
What should I do if I suspect cumulative toxicity?
Don’t stop your medication suddenly. Make an appointment with your doctor or pharmacist. Bring your medication log. Ask for specific tests: liver enzymes, kidney function, thyroid levels, EKG (for heart drugs), or lung function (if you’re on amiodarone). If your doctor dismisses your concerns, ask for a referral to a clinical pharmacist or toxicology specialist.





Donna Peplinskie
January 3, 2026 at 09:05
Wow, this post really hit home for me. I’ve been on amiodarone for six years, and my cardiologist never mentioned cumulative toxicity until I started having breathing issues. Now I’m on a waiting list for a lung specialist. I wish I’d known sooner. I keep a log now-every pill, every date. It’s scary how little we’re told.
Thank you for writing this. I’m sharing it with my support group.
Also, if anyone’s on lithium or digoxin, please, please ask your doctor for a thyroid and kidney panel. It’s not just about blood levels.
And yes, pharmacists are lifesavers. My pharmacist caught a dangerous interaction I didn’t even know about. We need more of them involved.
Don’t wait until you’re gasping for air.
- Donna