Most people assume that when they take a pill, the only thing that matters is the active ingredient-the drug itself. But what if the other 90% of that pill? The fillers, binders, colors, and coatings? What if those so-called ‘inactive’ ingredients aren’t so inactive after all?
What Exactly Are Excipients?
Excipients are the non-active components in medications. They make up 60% to 99% of a pill’s total weight. Think of them as the support crew for the active drug. They help the medicine hold its shape, dissolve properly in your stomach, taste less awful, or stay stable on the shelf. Common ones include lactose (a milk sugar), microcrystalline cellulose (ground wood pulp), magnesium stearate (a lubricant), and croscarmellose sodium (a disintegrant that helps the pill break apart).For decades, regulators and manufacturers treated these ingredients as harmless bystanders. The FDA calls them ‘inactive’ because they’re not meant to treat disease. But that label is starting to look outdated.
When ‘Inactive’ Isn’t Really Inactive
A 2020 study in Science shook up the pharmaceutical world. Researchers tested 314 common excipients against 44 biological targets-and found that 38 of them had measurable activity in the body. Some, like aspartame and sodium benzoate, blocked enzymes involved in brain chemistry. Propylene glycol, used in many liquid meds, interfered with an enzyme that breaks down neurotransmitters. And here’s the kicker: at normal doses, these excipients reached concentrations in the body that matched the levels shown to be biologically active in the lab.This isn’t theoretical. People with sensitivities already report reactions to excipients: headaches from tartrazine (a yellow dye), stomach upset from lactose, or rashes from certain preservatives. These aren’t allergies in the classic sense-they’re pharmacological interactions. Your body isn’t rejecting a foreign protein; it’s responding to a compound that’s quietly altering your biochemistry.
Why Generic Drugs Might Not Be the Same
If you’ve ever switched from a brand-name drug to a generic, you might have noticed a difference in how it works-or how you feel after taking it. That’s not just in your head. Generics are allowed to use different excipients as long as they don’t change the drug’s absorption or safety. But that’s a big ‘if’.The FDA requires identical excipients for injectables, eye drops, and ear drops. For pills? Not so much. A generic version of a blood pressure pill might swap out sodium starch glycolate for croscarmellose sodium as a disintegrant. Sounds minor, right? But in one case, Aurobindo’s generic version of Entresto was rejected because the new excipient changed how fast the drug dissolved at stomach pH-by 15%. That’s enough to affect how much drug gets into your bloodstream.
And it’s not just about absorption. Some excipients can trigger immune responses. In 2018, 14 generic valsartan products were recalled because a new solvent used in manufacturing created a cancer-causing contaminant, NDMA. That wasn’t the active ingredient-it was a byproduct of a new excipient process.

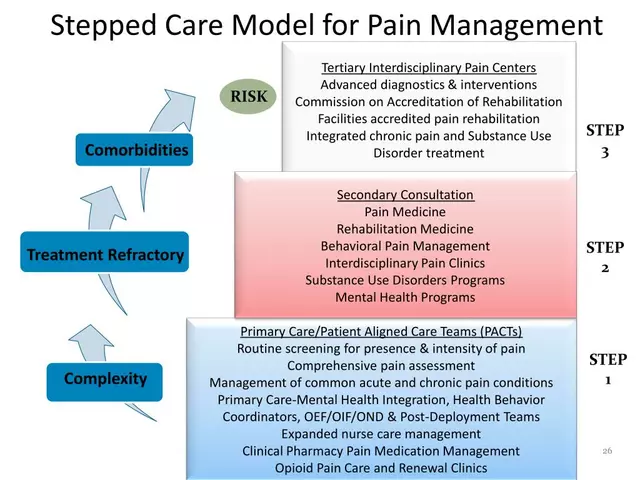
Regulatory Gaps and Real-World Risks
The FDA’s Inactive Ingredient Database lists around 1,500 approved excipients, with concentration limits for each route of administration. For example, polysorbate 80 is safe up to 5% in pills but capped at 0.05% in IV drips. But here’s the problem: most of these limits were set decades ago, based on toxicity studies in animals-not human biological interactions.Generic drug makers often rely on ‘prior safe use’ to justify new formulations. If an excipient was used in another approved drug, they assume it’s fine. But that ignores individual differences. Someone with a rare genetic variation in liver enzymes might process propylene glycol differently. A child might react to a dye that an adult tolerates. And with the rise of complex drugs-extended-release pills, combination therapies, or oral disintegrating tablets-the old rules don’t always apply.
That’s why 17% of generic drug applications get rejected-not for the active ingredient, but for excipient issues. The most common reasons? Not enough safety data on a new excipient (42%), or using a concentration that’s too high (38%).
What’s Being Done About It?
The FDA is finally catching up. In 2023, they proposed updating their database to include predicted tissue concentrations for each excipient-so they can see if a compound builds up in the liver, brain, or kidneys. They’re also running a pilot program requiring extra safety data for 12 high-risk excipients in orally disintegrating tablets, including aspartame and saccharin, after reports of rare hypersensitivity reactions.Researchers are building computational models to predict which excipients might interact with which biological targets. The goal? To screen new excipients before they ever hit a pill bottle. But that’s expensive. One estimate says adding a 50-target screening panel could add $500,000 to $1 million to the cost of developing a new generic drug.
Meanwhile, industry groups like PhRMA argue that excipient-related adverse events are extremely rare-only 0.03% of reports in the FDA’s database are definitively linked to excipients. That’s true. But that number doesn’t capture the subtle, chronic effects: fatigue, brain fog, or digestive changes that patients might never connect to their meds.
What This Means for You
You don’t need to panic every time you get a different-looking pill. For most people, excipients are harmless. But if you’ve noticed changes after switching brands-worse side effects, reduced effectiveness, new symptoms-it’s worth asking your pharmacist or doctor.Ask: ‘Is this generic using the same excipients as the brand?’ If they don’t know, request the manufacturer’s product insert. Look up the excipients online. If you see aspartame, tartrazine, or lactose-and you have sensitivities-ask if there’s an alternative formulation.
It’s not about avoiding generics. It’s about being informed. Your medication isn’t just the active ingredient. It’s the whole package. And that package? It’s more complex than you were told.
How to Check Your Medication’s Ingredients
You can find the full list of excipients on the drug’s package insert or by searching the FDA’s Inactive Ingredient Database. Here’s how:- Find the brand or generic name of your medication.
- Go to the FDA’s Inactive Ingredient Search tool (available online).
- Search by the drug’s name or active ingredient.
- Review the excipients listed for your route of administration (oral, injectable, etc.).
- Look up any unfamiliar ingredients-especially if you have known sensitivities.
Some common excipients to watch for if you’re sensitive:
- Lactose - Can cause bloating or diarrhea in those with lactose intolerance.
- Tartrazine (FD&C Yellow No. 5) - Linked to hyperactivity in children and rare allergic reactions.
- Aspartame - A sweetener that may affect neurotransmitter balance in sensitive individuals.
- Propylene glycol - Used in liquid meds; can cause irritation or metabolic effects at high doses.
- Magnesium stearate - A lubricant; some studies suggest it may slow drug absorption.
Future of Excipients: What’s Coming?
By 2025, experts predict that 30% of complex generic drug applications will require extra excipient safety testing-up from 18% in 2022. The push is coming from rising demand for personalized medicine, extended-release formulations, and combination pills. As these drugs get more sophisticated, so do the excipients needed to make them work.One emerging idea? Setting ‘inert thresholds’-concentrations below which an excipient is assumed to have no biological effect. But critics say that’s too simplistic. Everyone’s body is different. What’s safe for one person might trigger a reaction in another.
The bottom line? Excipients are no longer just filler. They’re part of the medicine’s story. And if you’re one of the people who feels ‘off’ on a generic, it might not be your imagination. It might be the ingredients you never knew were there.




Nicole M
November 13, 2025 at 04:47
Wow, I never thought about what’s in my pills beyond the drug name. I switched generics last year and started getting weird headaches-never connected it until now. Guess I’m checking my next prescription.