When a generic drug hits the market, you assume it works just like the brand-name version. But how do regulators know for sure? Traditional measures like partial AUC and Cmax used to be enough. Today, they’re often not. For complex drug formulations-especially extended-release pain meds, CNS drugs, or abuse-deterrent opioids-what happens in the first few hours after dosing can make or break safety and effectiveness. That’s where partial AUC comes in.
Why Traditional Bioequivalence Metrics Fall Short
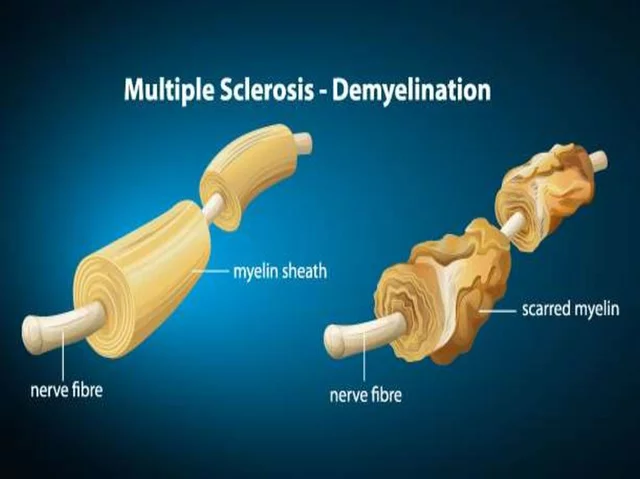
For decades, bioequivalence was judged using two numbers: Cmax (the highest concentration in the blood) and total AUC (the full area under the concentration-time curve). These told regulators whether the generic drug reached the same peak level and overall exposure as the original. Simple. Clean. But they missed the details.Imagine two painkillers: one releases all its drug at once, the other slowly over 12 hours. Both might have the same Cmax and total AUC. But if the generic spikes too fast, it could cause overdose. If it releases too slowly, it won’t relieve pain. Traditional metrics wouldn’t catch that. That’s not bioequivalence-it’s bioequivalence in name only.
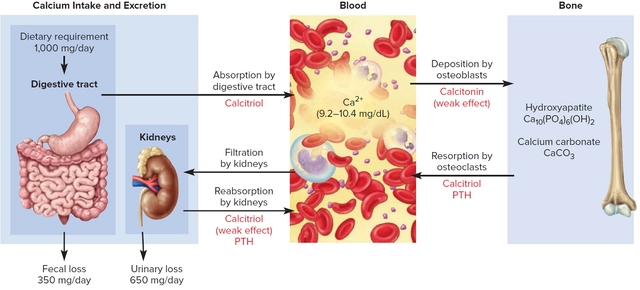
The European Medicines Agency (EMA) flagged this problem in 2013. Their draft guidance was the first to formally suggest using partial AUC for prolonged-release formulations. The U.S. FDA followed. By 2018, CDER launched a company-wide push to standardize pAUC use. Why? Because real patients weren’t getting the right dose at the right time.
What Is Partial AUC (pAUC)?
Partial AUC is not a new kind of measurement-it’s a smarter way to use the old one. Instead of looking at the entire drug exposure curve from zero to infinity, pAUC zooms in on a specific window: the time when absorption matters most.That window could be:
- The first 1-2 hours after dosing (when rapid absorption affects pain relief or seizure control)
- The time when drug concentration exceeds 50% of Cmax
- The period up to the Tmax (time to peak concentration) of the reference product
Regulators don’t pick these times randomly. They’re tied to clinical outcomes. For example, in abuse-deterrent opioids, early exposure must match the brand to prevent crushing or snorting from causing dangerous spikes. If the generic releases too quickly in that first hour, it defeats the whole purpose of the abuse-deterrent design.
Statistically, pAUC is analyzed the same way as total AUC: log-transformed, compared using ANOVA, and required to fall within the 80-125% confidence interval. But now, that interval applies to a slice of the curve-not the whole thing.
How pAUC Changed the Game for Generic Drugs
A 2014 study in the European Journal of Pharmaceutical Sciences showed something startling: among generic products that passed traditional bioequivalence tests, 20% failed when pAUC was applied. When both fasting and fed conditions were tested together, failure rates jumped to 40%.This wasn’t about poor manufacturing. It was about hidden differences in absorption kinetics. A generic might have the same total exposure, but if it absorbs slower in the first 90 minutes, patients might not get relief when they need it. In psychiatric drugs, that delay could mean a relapse. In epilepsy meds, it could mean a seizure.
One case presented at the 2021 AAPS meeting found a 22% difference in early exposure between a test and reference product. Total AUC was within limits. Cmax was fine. But pAUC over the first 2 hours showed the generic delivered 22% less drug during the critical absorption window. That product was pulled before it reached patients.
That’s the power of pAUC. It doesn’t just check if the drug gets in-it checks if it gets in when it needs to.

Where Is pAUC Used Today?
As of 2023, the FDA has mandated pAUC in over 127 product-specific guidances. The highest use is in three therapeutic areas:- Central nervous system drugs (68% of new submissions): Think ADHD meds, antiepileptics, antidepressants. Timing matters for brain chemistry.
- Pain management (62%): Especially extended-release opioids. Early exposure affects abuse potential and efficacy.
- Cardiovascular agents (45%): Blood pressure and heart rhythm drugs need steady levels. A delayed rise can cause dangerous fluctuations.
Even more telling: in 2022, 35% of all new generic drug applications included pAUC data. In 2015, that number was 5%. The trend is steep. By 2027, Evaluate Pharma predicts 55% of generic approvals will require pAUC.
The Hidden Costs and Challenges
pAUC isn’t easy. It’s expensive. It’s complex. And it’s inconsistent.A senior biostatistician at Teva told the ACPAC forum in 2022 that implementing pAUC for their extended-release opioid generic required increasing their study size from 36 to 50 subjects. That added $350,000 to development costs. But it prevented a clinical failure down the line.
Why the jump? pAUC metrics are more variable. The time to peak concentration differs between people. That variability means you need more participants to get statistically solid results. Some studies show sample sizes need to increase by 25-40% compared to traditional methods.
And then there’s the lack of standardization. FDA product-specific guidances vary wildly. Only 42% clearly define how to choose the pAUC time window. One guidance might say “use the first 2 hours,” another says “use up to 1.5× Tmax of the reference.” Developers are left guessing.
In 2022, the FDA rejected 17 ANDA submissions-8.5% of all bioequivalence-related deficiencies-because the pAUC time interval was poorly defined or unjustified. That’s not a technical glitch. It’s a design flaw.

Who Needs to Understand pAUC?
This isn’t just for regulators. If you work in generic drug development, you need to know pAUC. Job postings for bioequivalence specialists now list pAUC expertise as a requirement in 87% of cases (BioSpace, 2023). Biostatisticians typically need 3-6 months of extra training to get comfortable with the analysis.Tools like Phoenix WinNonlin and NONMEM are now standard. You can’t just run a t-test anymore. You need to model concentration-time profiles, define regions of interest, and justify your cutoffs based on pharmacodynamic data.
Smaller companies can’t afford in-house expertise. That’s why specialized CROs like Algorithme Pharma have grown. They now hold 18% of the complex generic bioequivalence market. Outsourcing pAUC analysis is no longer optional-it’s survival.
The Future of Bioequivalence
The FDA is working on solutions. In January 2023, they launched a pilot program using machine learning to predict optimal pAUC time windows based on reference product data. The goal? To reduce ambiguity and create standardized cutoffs across products.Meanwhile, the IQ Consortium reports that inconsistent pAUC rules between the FDA, EMA, and other agencies add 12-18 months to global generic drug development. That’s a huge delay for patients waiting for affordable medicines.
But the science is clear. As Dr. Bingming Wang of the FDA said in 2022: “For some products with complex PK profiles, the traditional metrics of AUC and Cmax may not be sufficient to ensure therapeutic equivalence.”
Partial AUC isn’t replacing total AUC. It’s supplementing it. It’s the missing layer of detail that turns a good generic into a safe, effective one.
By 2027, if a generic drug for a CNS or pain medication doesn’t include pAUC data, regulators won’t even look at it. The days of assuming “same total exposure = same effect” are over. The future belongs to precision pharmacokinetics.
What This Means for Patients
You don’t need to calculate a pAUC. But you should know this: the generic pill you take today is held to a higher standard than ever before. That extra testing isn’t red tape-it’s protection.For people on long-term pain meds, epilepsy drugs, or psychiatric treatments, a small timing difference in absorption can mean the difference between control and crisis. pAUC helps ensure that when you switch from brand to generic, your body gets the same drug, at the same rate, at the same time.
It’s not just science. It’s safety.



Jay Tejada
January 3, 2026 at 20:04
So basically, they’re now checking if the generic drug doesn’t turn into a speedball in the first hour? Kinda wild we didn’t do this sooner.