Tendon Rupture Risk Calculator
Risk Assessment Tool
This tool helps you understand your personal risk of tendon rupture when taking quinolone antibiotics and corticosteroids. Based on the U.S. FDA's warning that these drugs can increase tendon rupture risk by up to 46-fold when used together, this assessment considers key risk factors identified in clinical studies.
Your Risk Assessment
What to Do
Most tendon ruptures linked to quinolones occur after stopping the drug. If you experience:
- Deep ache or burning sensation in tendons
- Swelling or stiffness that worsens with movement
- Sudden pop or loss of function in a tendon
Stop the antibiotic immediately and contact your doctor. Early intervention can prevent rupture.
Imagine going for a morning walk, stepping off a curb, and hearing a loud pop in your heel. Suddenly, you can’t stand on that foot. No fall. No sports injury. Just a simple step - and your Achilles tendon is gone. For some people, this isn’t bad luck. It’s a known, preventable side effect of two common medications: quinolone antibiotics and corticosteroids.
What Are Quinolone Antibiotics?
Quinolone antibiotics - especially the fluoroquinolone subclass - are powerful drugs used to treat serious bacterial infections. Common examples include ciprofloxacin, levofloxacin, and norfloxacin. They work by attacking bacterial DNA, stopping infections from spreading. Because they’re taken orally and work well against a wide range of bacteria, they’ve been prescribed for decades for urinary tract infections, pneumonia, and sinus infections. But here’s the catch: they don’t just target bacteria. These drugs also interfere with human cells that produce collagen - the main protein in tendons. That’s why, even though they’re lifesaving in some cases, they come with a hidden danger: tendon damage.Why Tendons Are at Risk
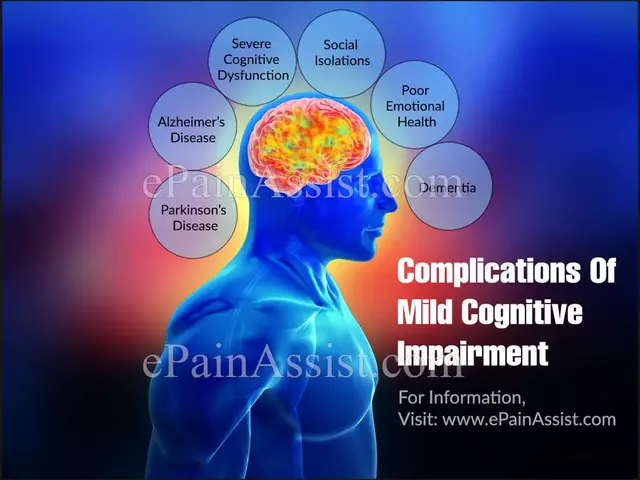
Tendons connect muscle to bone. They’re strong, but not flexible. They rely on healthy collagen fibers to handle stress. Quinolone antibiotics disrupt the way tendon cells (tenocytes) make and repair collagen. This doesn’t happen overnight. It starts subtly. You might feel a dull ache behind your ankle, or stiffness in your shoulder. It’s easy to ignore - maybe you overdid it at the gym, or slept funny. But if you’re also taking corticosteroids - like prednisone or methylprednisolone - the risk skyrockets. Corticosteroids break down collagen too. They’re used for inflammation, arthritis, asthma, and autoimmune conditions. When you combine them with a quinolone, you’re essentially attacking your tendons from two sides. A 2010 study in the Journal of the American Medical Association found that people taking both drugs had a 46-fold higher risk of Achilles tendon rupture than those taking neither. That’s not a small increase. That’s a red flag.Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain groups are far more vulnerable:- People over 60 - Tendons naturally weaken with age. Add a quinolone and steroid, and the chance of rupture jumps 2.7 times.
- Those on long-term steroids - Even low doses over weeks or months can thin tendons.
- People with kidney problems - Quinolones are cleared by the kidneys. If your kidneys aren’t working well, the drug builds up in your body, increasing toxicity.
- Diabetics - High blood sugar damages connective tissue, making tendons more fragile.
- Those who’ve had a prior tendon injury or transplant - Your body’s already compromised in that area.
When Does It Happen?
You might think the danger is only while you’re on the medication. But that’s not true. Half of all tendon ruptures linked to quinolones happen after you’ve stopped taking the drug. The median time to injury is just 6 days after starting the antibiotic - but symptoms can appear up to 6 months later. Many patients report pain or swelling in the tendon days or weeks before the rupture. It’s often described as a burning or deep ache, worse with movement. If you’re on a quinolone and feel this, don’t wait. Stop the drug and see your doctor. Early action can prevent a full rupture.Real Consequences, Long Recovery
A ruptured Achilles tendon isn’t just painful. It’s life-changing. Most cases require surgery. Recovery takes 6 to 12 months. You’ll need physical therapy, crutches, braces, and time off work. Many people never fully regain their previous strength or mobility. And about half of those affected have problems in both tendons - meaning both ankles could go out. In one study, 36% of reported cases weren’t just tendonitis - they were full ruptures. That’s not rare. That’s a pattern.
What Doctors Are Doing About It
In 2008, the U.S. FDA first warned about this risk. By 2013, they added a black box warning - the strongest possible - to all systemic fluoroquinolone labels. The message was clear: these drugs should not be used for mild infections like simple sinusitis or bronchitis. They’re reserved for life-threatening or hard-to-treat infections where no safer alternative exists. In Australia, New Zealand, and across Europe, regulators have issued similar alerts. Prescribers are now trained to ask: “Are you on steroids?” “Are you over 60?” “Do you have kidney issues?” If the answer is yes, they’re supposed to choose a different antibiotic. Still, these drugs are widely prescribed. Many patients don’t know the risk. Some doctors still reach for ciprofloxacin out of habit. That’s why patient awareness matters.What You Should Do
If your doctor prescribes a quinolone antibiotic:- Ask: “Is this the safest option for me?”
- Tell them if you’re taking any steroids - even a low-dose inhaler or joint injection.
- Ask about alternatives like amoxicillin, doxycycline, or trimethoprim.
- Watch for pain, swelling, or stiffness in your tendons - especially your heels, shoulders, or hands.
- If you feel sudden pain or hear a pop, stop the antibiotic immediately and get medical help.
The Bigger Picture
Quinolone antibiotics are not evil drugs. They’ve saved lives - especially in hospital-acquired infections or resistant strains. But medicine isn’t about using the strongest tool available. It’s about using the right tool for the right person. The combination of quinolones and corticosteroids is one of the clearest examples of a dangerous drug interaction that’s still overlooked. It’s not theoretical. It’s documented in tens of thousands of cases. It’s not rare. It’s predictable. And it’s preventable. If you’re older, on steroids, or have kidney disease - don’t let a quick fix for a urinary infection cost you your mobility. Ask questions. Push for alternatives. Your tendons will thank you.Can quinolone antibiotics cause tendon damage even after stopping the drug?
Yes. Up to half of all tendon ruptures linked to quinolone antibiotics occur after the patient has stopped taking the medication. The damage can develop slowly, and symptoms like pain or stiffness may appear days or even weeks after the last dose. This is why it’s critical to stay alert for tendon discomfort for up to six months after finishing treatment.
Which quinolone antibiotic has the highest risk of tendon rupture?
Ciprofloxacin is the most frequently reported quinolone associated with tendon rupture, accounting for nearly 68% of documented cases in major safety databases. Norfloxacin and levofloxacin also carry significant risk, but ciprofloxacin remains the most common culprit in clinical reports worldwide.
Are corticosteroid injections as risky as oral steroids when combined with quinolones?
Yes. Whether taken orally or injected - even as a single joint injection - corticosteroids suppress collagen production and weaken tendons. A single steroid injection combined with a quinolone antibiotic can still significantly raise the risk of rupture. There’s no safe threshold; the risk is cumulative.
Is tendon rupture from quinolones reversible?
Once a tendon ruptures, it cannot heal on its own without medical intervention. Surgery is often required, followed by months of rehabilitation. Even after recovery, many patients experience permanent weakness, reduced range of motion, or chronic pain. Prevention - not treatment - is the only reliable solution.
Should I avoid quinolone antibiotics completely if I’m over 60?
Not necessarily - but you should question their use. For serious infections like complicated UTIs, pneumonia, or anthrax exposure, quinolones may still be necessary. But for common issues like sinus infections, bronchitis, or uncomplicated UTIs, safer alternatives exist. Always ask your doctor: “Is this the best option for someone my age?”
What are the early warning signs of quinolone-induced tendinitis?
Early signs include localized pain, swelling, warmth, or stiffness in a tendon - especially the Achilles, shoulder, or wrist. The pain often worsens with movement and may feel like a deep ache or burning sensation. If you’re on a quinolone and notice this, stop the drug and contact your doctor immediately. Waiting until you can’t walk could mean a rupture.
Are there any safe alternatives to quinolone antibiotics?
Yes. For many infections, alternatives like amoxicillin-clavulanate, doxycycline, trimethoprim-sulfamethoxazole, or cefdinir are just as effective and carry no tendon rupture risk. The choice depends on the infection type, your allergies, and kidney function. Always discuss alternatives with your prescriber before accepting a quinolone.


Lance Nickie
January 13, 2026 at 05:28
cipro got me good. heard a pop walkin to the fridge. no gym, no fall. just... gone. doc said 'it happens' like it was normal. it's not.