Cancer Disparities: Why Some Groups Face Higher Risks and Fewer Options
When we talk about cancer disparities, differences in cancer rates, outcomes, and access to care across population groups. Also known as health inequities in oncology, it's not just about who gets diagnosed—it's about who survives, who gets treated early, and who gets left behind. Black Americans are 20% more likely to die from cancer than white Americans, even when diagnosed at the same stage. Native communities see higher rates of liver and stomach cancers tied to limited screening and delayed care. These aren’t random accidents—they’re the result of systems that have failed to keep up with who needs help most.
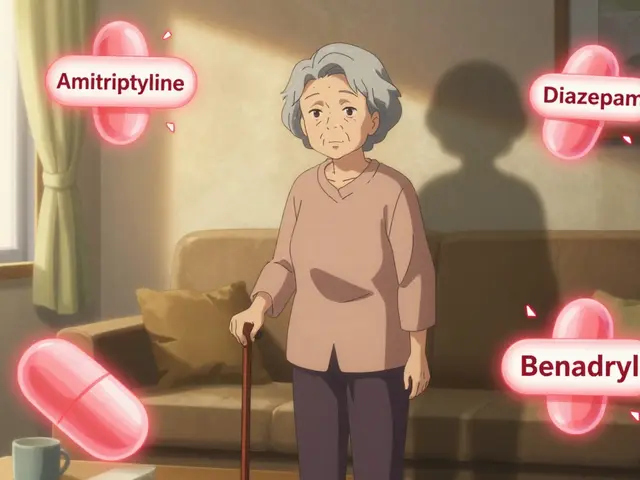
Access to cancer care, the ability to get timely diagnosis, treatment, and follow-up. Also known as healthcare access gaps, it’s broken in plain sight: a person in rural Appalachia might drive three hours just to see an oncologist, while someone in a wealthy suburb walks in the same day. Insurance coverage gaps, lack of transportation, and clinics that don’t accept Medicaid mean survival isn’t just about the tumor—it’s about your zip code, your job, and your skin color. Then there’s socioeconomic cancer risk, how income and education shape exposure to carcinogens and ability to prevent disease. Also known as poverty-linked cancer risk, it’s why low-income neighborhoods have more tobacco ads, fewer grocery stores with fresh food, and more pollution from nearby factories. These aren’t personal choices—they’re environmental traps. Even when treatments exist, cost becomes a barrier. A $10,000-a-month drug might work, but if your insurance denies it or your paycheck can’t cover the co-pay, it’s as good as invisible.
These gaps show up in every stage—from prevention to palliative care. Black women are more likely to die from breast cancer even though white women get diagnosed more often. Latino men have higher rates of prostate cancer but lower screening rates. Asian elders face language barriers that delay diagnosis. And LGBTQ+ patients often avoid care because they’ve been mistreated before. This isn’t about individual behavior. It’s about systems that ignore, underfund, or sideline entire communities.
What you’ll find here aren’t abstract theories or vague calls to action. These are real stories, real data, and real fixes—how genetic testing helps some but leaves others out, how pharmacy pricing hits marginalized groups hardest, how patient advocacy changes outcomes, and why the same drug can save one person and kill another based on their background. You’ll see how things like generic drug pricing, insurance negotiations, and even inactive ingredients in pills can widen the gap. This isn’t just about medicine. It’s about justice. And it’s time we treated it that way.
How Race and Ethnicity Affect Carcinoma Risk and Treatment Outcomes
Race and ethnicity significantly influence carcinoma risk, diagnosis timing, and treatment access. Learn how genetics, cultural barriers, and systemic bias affect outcomes-and what can be done to close the gap.
About
Health Conditions
Latest Posts

Why Real Customers Are Leaving CanadaDrugsDirect: Honest Stories & Alternatives
By Marcel Kornblum Apr 24, 2025

Tips for maintaining proper vaginal hygiene to prevent infections
By Marcel Kornblum Jun 26, 2023

Diclofenac Sodium and Muscle Pain: A Winning Combination?
By Marcel Kornblum May 16, 2023

