Every year, 36,000 older adults in the U.S. die from falls. That’s more than car crashes or gun violence in this age group. And it’s not just about slippery floors or poor lighting. The real culprit? Medications many seniors take every day without knowing the danger.
If you or someone you love is over 65 and taking more than three prescriptions, you’re not alone. Nearly half of older adults in the U.S. are on medications that silently raise their risk of falling - and many don’t even realize it. The problem isn’t just the number of pills. It’s which ones they are.
Which Medications Are Most Dangerous?
The American Geriatrics Society has a list of drugs they call fall risk-increasing drugs - or FRIDs. These aren’t rare or experimental. Most are common, prescribed for decades, and often taken long after they should be.
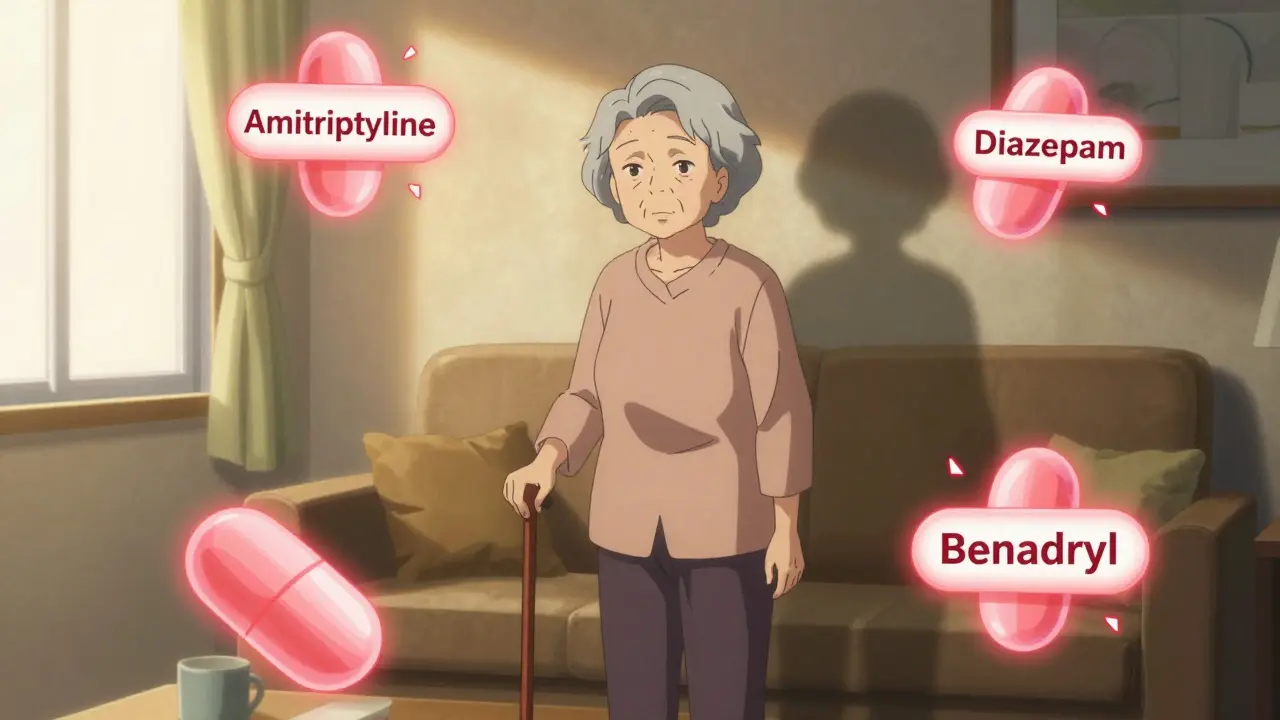
Antidepressants top the list. Not all of them, but tricyclics like amitriptyline and even common SSRIs like sertraline and fluoxetine have been shown to double fall risk in some studies. Why? They cause dizziness, low blood pressure, and slowed reaction times. One 2023 Mayo Clinic review found that older adults on antidepressants were 65% more likely to fall than those not taking them.
Benzodiazepines - drugs like Xanax, Valium, and Ativan - are another major offender. These are often prescribed for anxiety or sleep, but they don’t just make you sleepy. They dull your balance, blur your vision, and delay your reflexes. The risk isn’t just while you’re taking the pill. It lingers. A 72-year-old woman might take her nightly dose at 10 p.m., wake up at 3 a.m. to use the bathroom, and stumble because her body still hasn’t cleared the drug. Long-acting benzodiazepines like diazepam are especially risky. Short-acting ones like lorazepam are slightly better, but still dangerous over time.
Sedative-hypnotics like Ambien, Lunesta, and Sonata are often marketed as “safer” sleep aids. But they’re not. They cause complex sleep behaviors - walking, talking, or even driving while half-asleep. The CDC calls them “stealth fall risks.” One Reddit user shared that her 78-year-old mother fell three times in two months after starting Ambien. The third fall broke her hip. She never told her doctor the falls were linked to the medication.
Opioids - even low-dose ones - are another silent threat. They cause dizziness, confusion, and slowed breathing. High-potency opioids like oxycodone or fentanyl can increase fall risk by 80%, according to a 2023 JAMA Health Forum study. Many older adults take them for chronic back pain, thinking the trade-off is worth it. But the cost is balance, mobility, and sometimes life.
Then there are the ones you might not think of. Muscle relaxants like baclofen can increase fall risk by 70%. NSAIDs like ibuprofen and naproxen? They can drop your blood pressure when you stand up, leading to sudden dizziness. Even over-the-counter antihistamines for allergies - diphenhydramine (Benadryl), doxylamine - are anticholinergics. They cause dry mouth, blurred vision, and brain fog. A 2022 National Council on Aging survey found that 65% of older adults didn’t know their allergy meds could make them fall.
Why Do These Drugs Hurt More as We Age?
It’s not just that older people are frail. It’s that their bodies change. Kidneys and liver slow down. That means drugs stick around longer. A 25-year-old might process a dose of diazepam in 8 hours. A 75-year-old? It could take 24 hours or more. That means side effects last all day.
Also, older adults often take multiple drugs at once. This is called polypharmacy. And it’s not just about quantity - it’s about combinations. An antidepressant plus a benzodiazepine plus a blood pressure pill? That’s a perfect storm. The CDC says nearly 45% of older adults are on at least one “potentially inappropriate” medication, and most are on three or more. The risk of a fall doesn’t just add up - it multiplies.
And here’s the kicker: most older adults don’t know they’re at risk. A 2023 study in the Journal of Geriatric Physical Therapy found that 63% of seniors taking multiple fall-risk drugs had no idea any of them could make them stumble. Their doctors didn’t tell them. And they didn’t ask.

What Can Be Done?
The good news? You don’t have to live with this risk. There are proven ways to cut fall risk without giving up quality of life.
The CDC’s STEADI program - which stands for Stopping Elderly Accidents, Deaths & Injuries - recommends three simple steps: STOP unnecessary drugs, SWITCH to safer options, and REDUCE doses to the lowest effective level.
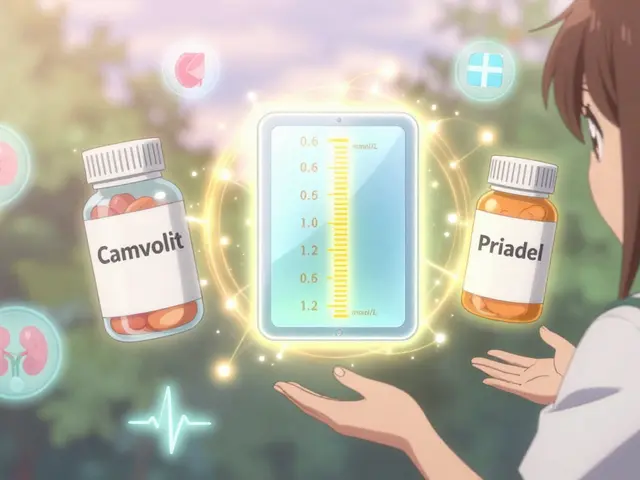
For sleep problems, cognitive behavioral therapy for insomnia (CBT-I) works better than sleeping pills. Studies show it’s 70-80% effective. For anxiety, therapy or low-dose buspirone can replace benzodiazepines. For pain, physical therapy, heat, or acetaminophen (in safe doses) are often safer than opioids or NSAIDs.
Pharmacists can help. A 2023 study showed that when a pharmacist reviews an older adult’s full medication list - including vitamins, supplements, and OTC drugs - fall risk drops by 22%. That’s why the “brown bag method” works: bring all your pills to your next appointment. Lay them out on the table. Ask: “Which of these could make me fall?”
Doctors should review medications at least once a year. But don’t wait for them to bring it up. Be the one to ask. Say: “I’ve been a little unsteady lately. Could any of my meds be causing that?”
Real Stories, Real Risks
One 81-year-old man took diazepam for anxiety and hydrocodone for arthritis. He’d been on both for 10 years. He never fell - until he did. He slipped in the bathroom, fractured his pelvis, and spent six months in rehab. His daughter later found out from his pharmacist that both drugs were on the Beers Criteria list for high fall risk. He was never warned.
Another woman, 76, took a daily dose of amitriptyline for nerve pain and a nightly dose of zolpidem for sleep. She started tripping over rugs. She thought it was her age. Her doctor didn’t connect the dots until she fell and broke her wrist. After stopping both drugs and switching to physical therapy and CBT-I, she regained her balance. She walks without a cane now.
These aren’t rare cases. They’re the rule.

What to Ask Your Doctor
If you’re over 65 and taking any prescription or OTC medication, ask these five questions:
- Is this medication still necessary? Could I stop it?
- Is there a safer alternative that doesn’t increase fall risk?
- Could this drug be interacting with another one I’m taking?
- Has this drug been reviewed for older adults? Is it on the Beers Criteria list?
- Can we try lowering the dose - even just a little - to see if I feel steadier?
Don’t be afraid to say: “I’m worried about falling. I want to make sure I’m not taking anything that could make that worse.”
It’s Not Just About Medicine
Medications are a big part of the problem - but not the whole story. Exercise, especially balance training like tai chi, cuts fall risk by nearly 50%. Home safety matters: remove throw rugs, install grab bars, add nightlights. Vision checks. Footwear with non-slip soles. All of it helps.
But if you’re taking a drug that makes you dizzy or slow, no amount of grab bars will fully protect you. The first step is always medication review.
The goal isn’t to eliminate every pill. It’s to eliminate the unnecessary ones. To replace dangerous ones with safer ones. To give older adults back their confidence - and their safety.
Because falling isn’t just an accident. For many, it’s the beginning of the end. And too often, it’s preventable - if we just look at the medicine cabinet.
What are the most dangerous medications for fall risk in older adults?
The most dangerous medications include antidepressants (especially tricyclics and SSRIs), benzodiazepines (like Xanax and Valium), sedative-hypnotics (like Ambien), opioids (especially high-dose ones), muscle relaxants (like baclofen), and anticholinergics (like Benadryl). These drugs cause dizziness, drowsiness, low blood pressure, or confusion - all of which impair balance and increase fall risk.
Can over-the-counter drugs cause falls in older adults?
Yes. Many OTC drugs like diphenhydramine (Benadryl), doxylamine (Unisom), and even some sleep aids and allergy pills are anticholinergics. They cause blurred vision, dry mouth, and brain fog - all of which increase fall risk. Studies show 65% of older adults don’t realize their allergy meds can make them unsteady.
How can I reduce my risk without stopping all my medications?
Start with a full medication review with your doctor or pharmacist. Ask if any drugs can be stopped, lowered in dose, or switched to safer alternatives. For sleep, try CBT-I instead of sleeping pills. For anxiety, consider therapy or buspirone. For pain, use physical therapy or acetaminophen. The CDC’s STEADI program recommends the three S’s: STOP unnecessary drugs, SWITCH to safer options, and REDUCE doses to the lowest effective level.
Is it safe to stop a medication like Xanax or Ambien on my own?
No. Stopping benzodiazepines or sleep medications abruptly can cause seizures, rebound insomnia, or severe anxiety. Always work with your doctor to taper off slowly - usually over 8 to 12 weeks. Never quit cold turkey. Your doctor can help you create a safe plan.
What should I bring to my doctor’s appointment to review my medications?
Bring every pill, capsule, liquid, patch, and supplement you take - including OTC drugs, vitamins, herbal remedies, and even eye drops. Use the “brown bag method”: put everything in a brown bag and show it to your doctor. This helps them spot duplicates, interactions, and high-risk drugs you may not realize you’re taking.



Michael Bond
December 25, 2025 at 18:30
My grandpa was on amitriptyline and Xanax for years. Never thought twice until he took a tumble in the shower. Turned out his doctor had prescribed both back in 2010 and never revisited them. We pulled the plug on both - slowly, with supervision - and he’s been walking without a cane since. Sometimes the simplest fix is just asking if a pill still needs to be there.