Eye Steroids: What You Need to Know
When dealing with eye steroids, potent anti‑inflammatory medicines applied directly to the eye. Also known as ocular steroids, they work by dampening the immune response that causes swelling and pain.
One major class of these drugs is corticosteroid eye drops, formulations such as prednisolone acetate or dexamethasone. They are prescribed for conditions like ocular inflammation, including uveitis, postoperative inflammation, and allergic conjunctivitis. While they can quickly restore clarity and comfort, they also carry a risk of increasing intra‑ocular pressure, which may lead to glaucoma, a serious optic nerve disease if not monitored. Proper prescription guidelines, dose, duration, and follow‑up eye exams are crucial to balance benefits and safety.
How Eye Steroids Work and When They're Used
Eye steroids encompass corticosteroid eye drops that suppress inflammatory cytokines, reduce vascular permeability, and stabilize cell membranes. They are required when the eye’s own defense mechanisms cause more harm than the original insult, such as after cataract surgery or in chronic uveitis. The typical prescription pattern involves a higher frequency at the start (e.g., one drop every hour) then tapering based on the physician’s assessment. This tapering process is a key part of the treatment plan because abrupt cessation can trigger a rebound flare‑up.
Patients should be aware that not every redness or irritation needs a steroid. For mild allergic reactions, antihistamine drops may be sufficient, and using a steroid unnecessarily could expose the eye to avoidable side effects. Monitoring intra‑ocular pressure is a standard part of the follow‑up schedule: an eye exam each week for the first month, then every few weeks as the dose drops. If pressure rises above 21 mm Hg, the doctor may add a pressure‑lowering medication or switch to a milder steroid.
Another practical tip is to avoid contact lenses while using steroid drops unless the doctor explicitly says it’s safe. The drops can leave residues that trap bacteria on the lens, raising infection risk. Also, patients should report any new visual disturbances, such as halos around lights, which could signal early glaucoma.
Below you’ll find a curated set of articles that dive deeper into specific eye steroid topics—everything from safety profiles of popular brands to step‑by‑step tapering schedules and how to spot early signs of pressure spikes. Use this collection to fine‑tune your understanding and manage your eye health with confidence.
How Steroids Manage Post‑Surgical Eye Inflammation - Complete Guide
Learn how steroids control eye inflammation after surgery, which drugs to use, proper dosing, side‑effects, monitoring, and safe alternatives in a clear, step‑by‑step guide.
About
Medications
Latest Posts


Testimonial for on-line pharmacy shop medsengage.com
By Marcel Kornblum Oct 27, 2023
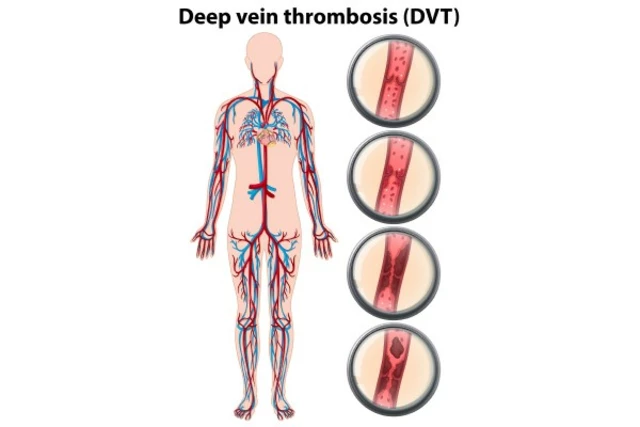
How to Reduce the Risk of Deep Vein Thrombosis During Long Flights
By Marcel Kornblum May 12, 2023

Eflornithine for Ingrown Hairs: How It Works and What to Expect
By Marcel Kornblum Oct 16, 2025

