Gene-Drug Interactions: How Your DNA Affects Medication Safety and Effectiveness
When you take a pill, your body doesn’t treat it the same way everyone else’s does. That’s because of gene-drug interactions, the way your genetic makeup changes how your body absorbs, breaks down, or responds to medications. Also known as pharmacogenomics, this field explains why one person might need a low dose of a drug to feel relief, while another needs triple that amount—or why someone might have a dangerous reaction to a common medicine that others tolerate just fine.
Your genes control the enzymes that process drugs. Some people have versions of these enzymes that work too fast, flushing the drug out before it can help. Others have enzymes that work too slow, letting the drug build up to toxic levels. This isn’t rare—it affects nearly everyone. For example, a gene called CYP2D6 determines how you process antidepressants, painkillers like codeine, and even some heart medications. If you’re a slow metabolizer, you might get sick from a standard dose. If you’re a super metabolizer, the drug might not work at all. That’s why two people with the same condition can have totally different outcomes on the same prescription.
These interactions aren’t just about side effects—they change how well treatment works. Take antiseizure drugs like lamotrigine or carbamazepine. Small changes in how your body absorbs them can trigger seizures if your genes affect liver enzymes. Or consider warfarin, a blood thinner. A single gene variation can mean the difference between a safe dose and a life-threatening bleed. Even supplements like evening primrose oil can interfere with antipsychotics if your genes alter how your brain handles neurotransmitters. And it’s not just about the drug itself—some inactive ingredients in pills can trigger reactions in people with certain genetic sensitivities.
Doctors rarely test for these gene-drug interactions before prescribing. But the data is out there. Studies show that up to 90% of people carry at least one genetic variant that affects how they respond to common medications. The good news? You don’t need to wait for a doctor to order a test. If you’ve ever had a medication fail you, caused unexpected side effects, or didn’t work even at high doses, your genes might be the reason. That’s why understanding gene-drug interactions is no longer just for researchers—it’s practical knowledge for anyone taking meds regularly.
Below, you’ll find real-world examples of how this plays out: from how race and genetics influence cancer treatment outcomes, to why generic antiseizure drugs can be risky for some, to how diet changes the way atomoxetine works in your brain. These aren’t abstract theories—they’re stories of real people whose lives changed once they understood their own biology. Whether you’re managing chronic pain, mental health, heart conditions, or just trying to avoid bad reactions, the answers are in your genes.
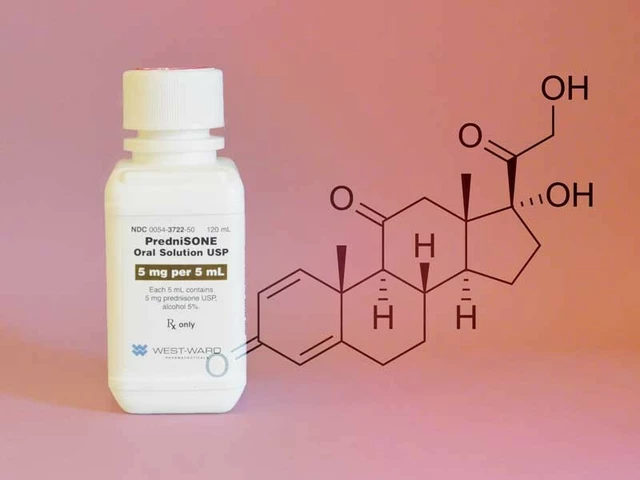
Preventing Adverse Drug Reactions with Pharmacogenetic Testing
Pharmacogenetic testing uses your DNA to predict how you'll react to medications, preventing dangerous side effects. Studies show it cuts adverse drug reactions by 30%, making treatment safer and more effective.
About
Medications
Latest Posts


The power of art in AIDS activism: How creativity can inspire change
By Marcel Kornblum Aug 1, 2023

Exploring Effective Alternatives to Flagyl for Diverse Infections
By Marcel Kornblum Feb 4, 2025

The Link Between Depression and Suicide: Warning Signs and Prevention
By Marcel Kornblum Jul 21, 2023