Understanding Heart Failure: A Practical Overview
When talking about Heart Failure, a chronic condition where the heart cannot pump enough blood to meet the body’s needs. Also known as cardiac insufficiency, it affects millions worldwide and shows up in many forms, from sudden breathlessness to subtle fatigue. Knowing what heart failure really means sets the stage for everything else you’ll read here.
One of the first concepts linked to heart failure is Ejection Fraction, the percentage of blood the left ventricle pushes out with each beat. A normal ejection fraction sits around 55‑70%, but many heart‑failure patients see it dip below 40%, signaling reduced pumping ability. This metric helps doctors decide whether a patient has systolic dysfunction, a key sub‑type of heart failure.
Core Treatments and How They Fit Together
Effective management of heart failure requires a toolbox of medicines. ACE Inhibitors, drugs that relax blood vessels and lower the heart’s workload are often the first line because they improve ejection fraction and slow disease progression. Another cornerstone is Beta Blockers, medications that blunt the heart’s response to stress hormones. By dampening heart rate, they reduce oxygen demand and prevent harmful remodeling of cardiac tissue.
Diuretics round out the regimen. These “water pills” help eliminate excess fluid, easing swelling in the legs and breathing difficulties. When patients follow a structured plan that includes ACE inhibitors, beta blockers, and diuretics, the odds of hospitalization drop dramatically. This triple‑therapy approach illustrates the semantic triple: Heart failure requires ACE inhibitors, beta blockers, and diuretics for optimal control.
Beyond meds, lifestyle tweaks matter. Low‑sodium diets, regular low‑impact exercise, and weight monitoring empower patients to stay ahead of fluid buildup. The New York Heart Association (NYHA) classification—ranging from Class I (no limitation) to Class IV (severe limitation)—helps clinicians tailor advice based on how daily activities are affected.
Technology also plays a role. Remote monitoring of weight and blood pressure can flag early signs of decompensation, giving doctors a chance to adjust therapy before an emergency visit. In many cases, a simple daily weigh‑in saves a hospital stay.
While the medical side is critical, emotional support shouldn’t be overlooked. Living with heart failure can be stressful, and anxiety often worsens symptoms. Counseling, support groups, and clear communication with caregivers boost adherence to treatment plans and improve quality of life.
Research continues to push the boundary. New classes like ARNIs (angiotensin receptor‑neprilysin inhibitors) and SGLT2 inhibitors, originally diabetes drugs, now show clear benefits for heart‑failure patients, even those with preserved ejection fraction. This evolving landscape means staying updated can make a real difference.
All of these pieces—ejection fraction, medication classes, lifestyle changes, and emerging therapies—interlock to form a comprehensive strategy for managing heart failure. Below you’ll find a curated list of articles that dive deeper into each topic, offering evidence‑based tips and real‑world advice to help you take control of your heart health.
Sacubitril for Heart Failure in HIV/AIDS Patients: Promise and Evidence
Explore how sacubitril, part of the ARNI class, may improve heart failure outcomes in HIV/AIDS patients, covering mechanisms, trial data, dosing, and safety.
About
Medical Research
Latest Posts


Why Storax is the Ultimate Game-Changer in Dietary Supplements
By Marcel Kornblum May 20, 2023

Unlock the Power of Calcium D-Glucarate: The Ultimate Dietary Supplement for Health
By Marcel Kornblum Mar 17, 2025
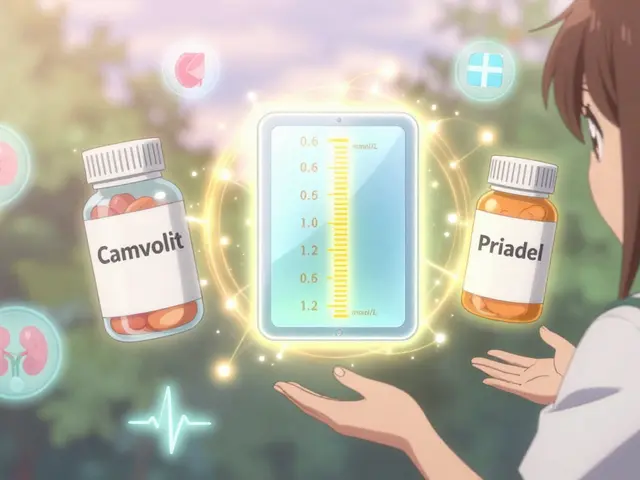
Lithium Carbonate Generics: What You Need to Know About Serum Levels
By Marcel Kornblum Jan 11, 2026

