When someone says they’re just "trying to eat healthier," it’s easy to miss the warning signs. But behind that phrase, for many, lies a life-consuming battle with food, weight, and self-worth. Eating disorders aren’t phases. They aren’t vanity. They’re serious, life-threatening illnesses that affect more people than most realize - and far too few get the right help in time.
What Anorexia and Bulimia Really Look Like
Anorexia nervosa isn’t just about being thin. It’s a mental illness where the brain locks into a fear of gaining weight, no matter how underweight a person becomes. People with anorexia often restrict food to extreme levels, exercise obsessively, or both. Their body weight falls far below what’s medically safe - sometimes below a BMI of 15. But here’s the part no one talks about: less than 6% of people with eating disorders are classified as "underweight" by medical standards. That means most sufferers don’t fit the stereotype. They might look fine to you. But inside, their body is shutting down. Bulimia nervosa looks different. People with bulimia cycle between binge eating - consuming large amounts of food in a short time, often in secret - and then trying to undo it. Purging methods include vomiting, using laxatives, fasting, or over-exercising. One in ten people with bulimia end up with swollen cheeks from repeated vomiting, a sign their body is under constant stress. Unlike anorexia, people with bulimia often maintain a normal or slightly above-normal weight, which makes it even harder to spot. Both disorders come with terrifying physical consequences. Anorexia has the highest death rate of any mental illness. One person dies from an eating disorder every 52 minutes in the U.S. alone. The heart weakens. Bones crumble. Organs fail. Bulimia damages the esophagus, causes electrolyte imbalances that can trigger cardiac arrest, and leads to chronic dehydration. And it’s not just the body - the mind is in crisis too. About 31% of people with anorexia and 23% with bulimia have attempted suicide. The risk is 18 times higher than for someone without an eating disorder.Why Most Treatments Fail - And What Actually Works
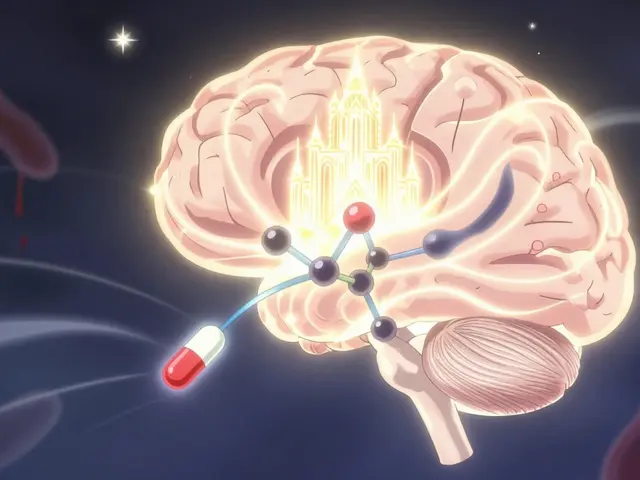
Too often, people with eating disorders are sent to general therapists who don’t know how to treat them. Or they’re told to just "eat more." That’s like telling someone with a broken leg to walk it off. The truth is, eating disorders require specialized care - not just talk therapy, but medical, nutritional, and psychological support all at once. For adolescents with anorexia, the gold standard is Family-Based Treatment (FBT). It puts parents - not therapists - in charge of restoring their child’s weight. The family eats meals together, monitors food intake, and gradually returns control to the teen as recovery progresses. Studies show 40-50% of teens recover fully after 12 months with FBT. Compare that to individual therapy alone, which helps only 20-30%. For adults with bulimia or binge eating disorder, Enhanced Cognitive Behavioral Therapy (CBT-E) is the most effective approach. It doesn’t just focus on food. It targets the core beliefs: "I’m worthless if I gain weight," "My body is my enemy," "If I don’t control this, I’ll lose control of everything." In 20 sessions, CBT-E helps 60-70% of people stop bingeing and purging. And it works across diagnoses - whether it’s bulimia, binge eating, or even atypical anorexia. The key? Starting early. If treatment begins within three years of symptoms appearing, remission rates jump to 65%. And now, for the first time, there’s a medication approved specifically for an eating disorder. In 2023, the FDA approved lisdexamfetamine (Vyvanse) for binge eating disorder. In clinical trials, it cut binge episodes by over 50% compared to placebo. It’s not a cure, but it’s a tool - especially for people who haven’t responded to therapy alone.
The Hidden Crisis: Insurance, Waitlists, and Broken Systems
Even when people know what they need, the system often blocks them. In 2022, 68% of people surveyed by the National Eating Disorders Association reported at least one insurance denial for treatment. One woman spent 27 months waiting - nine months for outpatient therapy, another 18 for an intensive program - because her insurance kept rejecting coverage. Another person raised $78,000 on GoFundMe to pay for 90 days of residential care after her insurance denied it 11 times. There are only about 1,200 specialized treatment beds in the entire U.S. for 30 million people with eating disorders. That’s less than 0.004% of those who need help getting access each year. In rural areas, 78% of counties have zero eating disorder specialists. A 2023 Johns Hopkins study found that if you live outside a major city, your chances of getting timely care are nearly zero. And even when you get in, the quality varies wildly. Only 38% of treatment centers meet basic standards for clinical documentation. Only 12% track outcomes using tools like the Eating Disorder Examination Questionnaire (EDE-Q). That means many patients are being treated without knowing if the treatment is working.What Recovery Really Feels Like - Real Stories
One user on HealthUnlocked shared: "After seven years of bulimia, I finally got CBT-E through a university clinic. In 12 sessions, my binge-purge episodes dropped from 14 times a week to two." Another, in a residential program at Monte Nido, said: "I gained 15 pounds under medical supervision. I learned DBT skills. For the first time in years, I didn’t hate my body." But recovery isn’t linear. Relapse is common. And the shame doesn’t vanish overnight. Many people spend years rebuilding trust in their bodies - learning to eat without guilt, to move without punishment, to exist without measuring their worth in calories.
How to Help - If You or Someone You Know Is Struggling
If you suspect someone has an eating disorder, don’t wait for them to "look sick." Don’t comment on their weight. Don’t say "you’re too thin" or "you’re not eating enough." Instead, say: "I’ve noticed you’ve been really stressed around meals lately. I care about you, and I’m here if you want to talk." If you’re the one struggling, reach out - even if it’s just to a school counselor, a doctor, or a hotline. The National Eating Disorders Association offers free, confidential screening tools at nationaleatingdisorders.org. You don’t need to be "bad enough" to deserve help. For clinicians: Learn FBT or CBT-E. Get trained. The Learning Curve Assessment Tool says you need 120-180 hours of specialized training to do this right. Don’t guess. Don’t wing it. Lives depend on it.The Road Ahead
There’s hope. The NIH is spending $25 million to track 7,500 children from birth to adolescence, looking for early biological signs of eating disorders. Telehealth is expanding - and could cut wait times by 40% by 2027. New laws are forcing insurance companies to cover treatment fairly. In 2023, the Department of Labor fined 17 health plans $3.2 million for denying eating disorder care. But progress is slow. The number of children under 12 being hospitalized for eating disorders rose 119% between 2012 and 2021. Teen prevalence is now at 6-8%. We’re seeing more cases, faster, and with more severity. The question isn’t whether we can fix this. It’s whether we’ll act before another 10,200 people die this year.Is anorexia only a problem for teenage girls?
No. While anorexia is more common in young females, diagnosis in males has been rising. About 1 in 4 people with anorexia are male. It also affects adults - including people in their 40s and 50s - and even children under 12. The stereotype of a thin teenage girl is outdated and dangerous because it delays diagnosis in others.
Can someone have an eating disorder and still be a normal weight?
Absolutely. In fact, less than 6% of people with eating disorders are medically classified as underweight. People with bulimia, binge eating disorder, or atypical anorexia can be normal weight or overweight. The diagnosis is based on behaviors and thoughts - not weight alone. Judging someone by their appearance can prevent them from getting help.
Is therapy enough to treat an eating disorder?
Not on its own. Eating disorders damage the body physically. You can’t fix a heart that’s beating too slowly or bones that are crumbling with talk therapy alone. Effective treatment requires medical monitoring, nutritional rehabilitation, and psychological therapy together. For adolescents with anorexia, Family-Based Treatment is the only first-line approach proven to work. For adults with bulimia, CBT-E is the most effective.
Why do insurance companies deny eating disorder treatment so often?
Because they treat it as a lifestyle issue, not a medical one. Many insurers still classify eating disorders as "behavioral" or "elective," even though they cause organ failure, electrolyte imbalances, and cardiac arrest. The Mental Health Parity and Addiction Equity Act (MHPAEA) requires equal coverage for mental and physical health - but enforcement is inconsistent. In 2023, the Department of Labor fined insurers $3.2 million for violating this law.
What’s the best way to support someone recovering from an eating disorder?
Don’t focus on food or weight. Don’t praise them for eating "good" foods or losing weight. Instead, focus on their feelings. Ask: "How are you feeling today?" or "What do you need right now?" Offer to sit with them during meals if they’re comfortable. Avoid giving advice unless asked. Recovery is about rebuilding trust - in food, in their body, and in others. Your steady, non-judgmental presence matters more than any solution you offer.
Is recovery possible after years of having an eating disorder?
Yes. While early treatment leads to better outcomes, recovery is possible at any stage. People in their 30s, 40s, and even 50s have successfully recovered from long-term anorexia and bulimia. The key is finding the right treatment - especially CBT-E or FBT - and having consistent support. Recovery isn’t about becoming perfect. It’s about learning to live without the disorder controlling your life.




Rich Robertson
December 15, 2025 at 07:04
Been there. Not even close to underweight. Looked fine. Still got hospitalized. No one believed me until my heart started skipping beats. It’s not about being skinny-it’s about the voice in your head screaming you’re not enough.
They gave me a meal plan. Didn’t fix the shame. Took years to unlearn that food = failure.