IBD Pregnancy: What You Need to Know About Managing Inflammatory Bowel Disease During Pregnancy
When you have Inflammatory Bowel Disease, a group of chronic digestive conditions including Crohn’s disease and ulcerative colitis that cause inflammation in the gut. Also known as IBD, it affects how your body digests food, absorbs nutrients, and handles inflammation. For many women, the biggest question isn’t just how to control symptoms—it’s how to stay healthy while carrying a baby. The good news? Most women with IBD can have safe, successful pregnancies. But it takes planning, the right team, and knowing which medications are safe to keep using.
One of the biggest concerns is medication safety during pregnancy, whether the drugs used to control IBD could harm fetal development or trigger complications. Many common IBD treatments, like mesalamine and certain biologics, are considered low-risk based on years of real-world data. But others, like methotrexate, are dangerous and must be stopped months before trying to conceive. It’s not about avoiding meds entirely—it’s about choosing the right ones. Studies show that uncontrolled IBD flares during pregnancy carry more risk to the baby than most medications do. Keeping your disease in check helps prevent preterm birth, low birth weight, and other complications.
Then there’s Crohn’s disease, a type of IBD that can affect any part of the digestive tract and often causes deep inflammation, ulcers, and strictures, versus ulcerative colitis, a form of IBD limited to the colon and rectum, causing surface inflammation and bleeding. While both need careful management, their impact on pregnancy can differ. Women with Crohn’s may face higher risks of flare-ups during the first trimester or postpartum, while those with ulcerative colitis often see improvement during pregnancy—though flare-ups can still happen. Nutrition becomes even more critical. Weight gain, iron levels, and vitamin D aren’t just about feeling better—they’re tied directly to fetal growth and long-term health.
It’s not just about drugs and diagnosis. The emotional side matters too. Stress doesn’t cause IBD, but it can make flares worse. Sleep gets hard. Doctor visits multiply. And the fear of passing something on to your child? Real. That’s why support systems, clear communication with your gastroenterologist and OB-GYN, and knowing your options make all the difference. You’re not alone—thousands of women have walked this path before you.
Below, you’ll find real, practical advice from people who’ve been there. From how to talk to your doctor about staying on your current meds, to what to expect when switching treatments, to how to track your symptoms without getting overwhelmed—these articles give you the tools to take control. No fluff. No guesswork. Just what works.
IBD and Pregnancy: Safe Medications and Fetal Risks Explained
Learn which IBD medications are safe during pregnancy, which to avoid, and how to plan ahead for a healthy pregnancy. Uncontrolled IBD poses greater risks than most treatments.
About
Health Conditions
Latest Posts
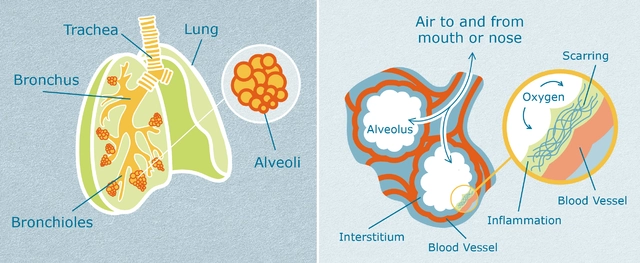
The Impact of Idiopathic Pulmonary Fibrosis on Relationships and Social Life
By Marcel Kornblum Apr 30, 2023
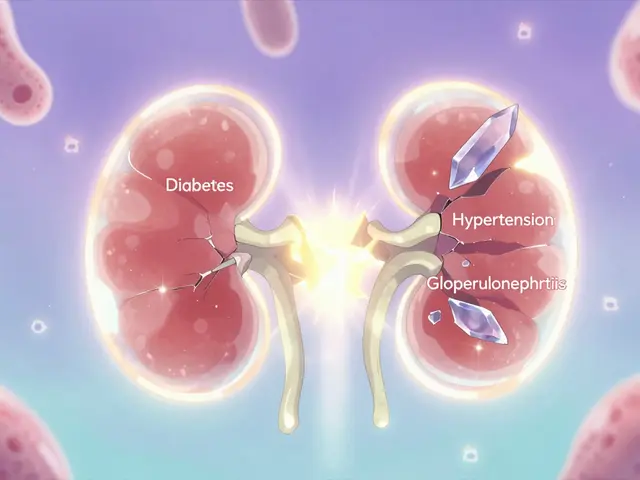
Kidney Failure Causes: How Diabetes, Hypertension, and Glomerulonephritis Damage Your Kidneys
By Marcel Kornblum Jan 7, 2026

How Steroids Manage Post‑Surgical Eye Inflammation - Complete Guide
By Marcel Kornblum Oct 13, 2025

