NTI Drugs: What They Are, Why They Matter, and What You Need to Know
When you take a medication, you expect it to work—without too much risk. But with NTI drugs, medications with a narrow therapeutic index where the difference between a helpful dose and a dangerous one is very small. Also known as narrow therapeutic index drugs, these are not like regular prescriptions. They demand precision—too little and they don’t work; too much and they can land you in the hospital. Think warfarin, lithium, digoxin, or phenytoin. These aren’t just any pills. They’re like walking a tightrope: one misstep, and things go wrong fast.
Why does this matter? Because generic versions, lower-cost copies of brand-name drugs that must meet strict bioequivalence standards for NTI drugs. Also known as therapeutic equivalents, are held to higher standards than usual. A small change in how your body absorbs the drug—because of different fillers, coatings, or manufacturing—can throw off your whole treatment. That’s why switching from one brand to another, even if labeled "generic," can be risky with NTI drugs. Your doctor or pharmacist should always check if the switch is safe. And if you’re on one of these meds, never swap pills without talking to your care team.
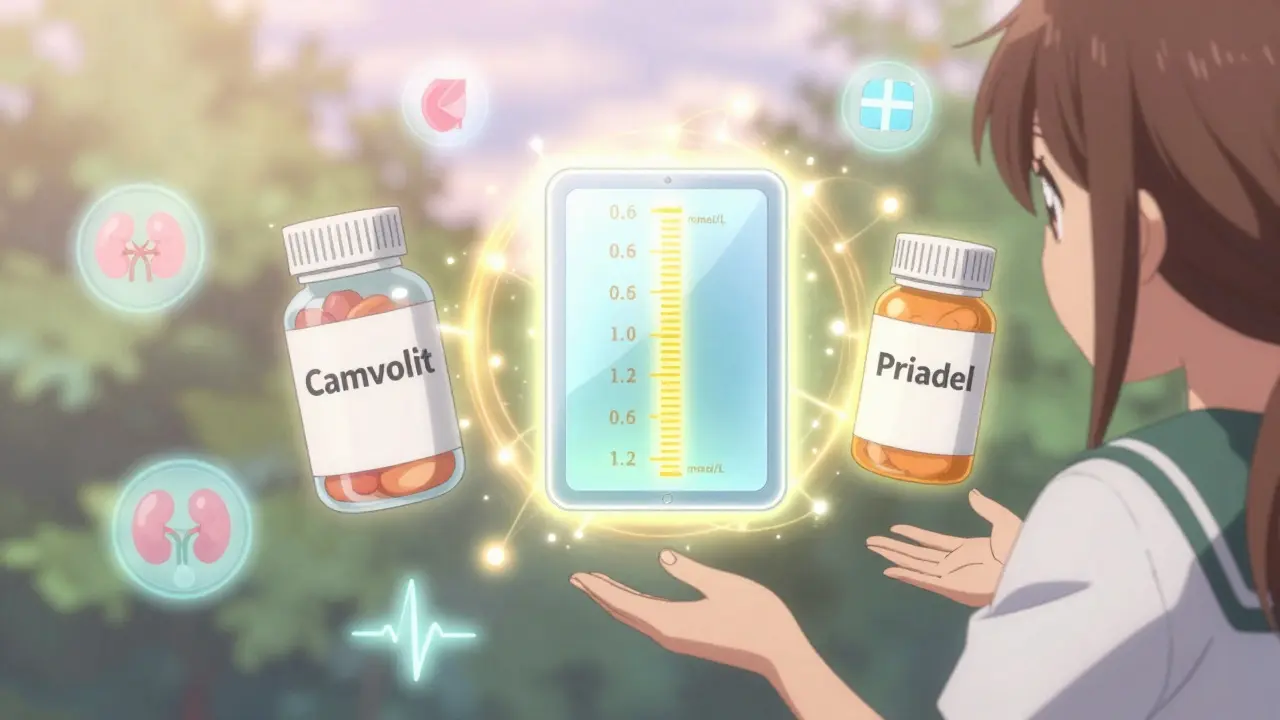
Drug monitoring, the regular blood tests used to track levels of NTI drugs to ensure they stay within the safe range. Also known as therapeutic drug monitoring, is often required. It’s not optional. If you’re on lithium, for example, your blood level needs checking every few months—or more often if your dose changes. Same with warfarin: your INR has to be just right. Too high, and you risk bleeding. Too low, and you could have a stroke. These aren’t "set it and forget it" meds. They need attention. And that’s why the posts below cover real-world issues: how excipients in generics might affect absorption, how diet can change how atomoxetine works, or why switching antifungals or antibiotics requires careful planning. All of it ties back to one truth: with NTI drugs, the details matter more than you think.
You’ll find guides here on comparing similar drugs—like cyclosporine vs. tacrolimus, or Zyvox vs. other antibiotics—because even small differences in how these drugs behave can be critical. You’ll see advice on managing side effects, understanding interactions, and avoiding dangerous switches. These aren’t theoretical discussions. They’re based on real cases where people got hurt because no one paid attention to the fine print. If you’re taking an NTI drug—or care for someone who is—this collection gives you the tools to ask the right questions, spot red flags, and stay in control.
Lithium Carbonate Generics: What You Need to Know About Serum Levels
Lithium carbonate generics require careful serum level monitoring due to their narrow therapeutic index. Switching brands can change your blood levels - even if the dose stays the same. Learn what targets to aim for, how often to test, and why vigilance matters.
Antiseizure Medications and Generic Substitution: Risks and Best Practices
Generic antiseizure medications can save money, but for NTI drugs like lamotrigine and carbamazepine, even small changes in absorption can trigger seizures. Learn the risks, who’s most vulnerable, and how to protect your treatment.
About
Medications
Latest Posts


Best Safe Alternatives to Amoxicillin: Expert Guide on Switching Antibiotics
By Marcel Kornblum May 24, 2025

When to take cefixime: understanding the best time for antibiotic treatment
By Marcel Kornblum Apr 27, 2023

Acamprosate vs Alternatives: Which Alcohol‑Dependence Medication Works Best?
By Marcel Kornblum Sep 26, 2025