Ocular Inflammation Treatment – What You Need to Know
When dealing with ocular inflammation treatment, the medical approach to reduce swelling, pain, and vision risk inside the eye. Also known as eye inflammation therapy, it blends drugs, monitoring, and sometimes surgery to keep the eye healthy. Ocular inflammation treatment isn’t one‑size‑fits‑all; it changes based on the cause, severity, and patient needs.
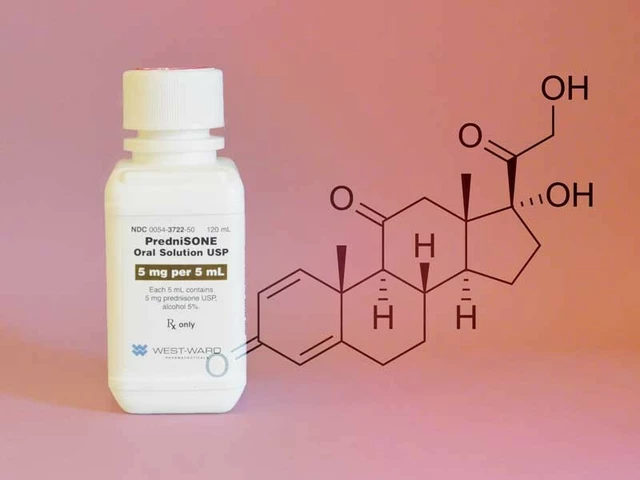
One of the most common pillars is corticosteroids, potent anti‑inflammatory agents that block multiple inflammatory pathways. They’re the go‑to for acute flare‑ups because they quickly calm the immune response and protect vision. However, long‑term use can raise eye pressure or cause cataracts, so doctors often look for alternatives once the storm settles.
When steroids alone aren’t enough or cause side effects, immunosuppressants, medications that dampen the immune system’s activity step in. Drugs like methotrexate or mycophenolate target the underlying immune drivers, making them useful for chronic conditions such as uveitis. They require regular blood tests, but they can spare patients from high steroid doses.
In recent years, biologics, targeted therapies that block specific cytokines or immune cells have reshaped the landscape. Agents such as adalimumab zero in on tumor necrosis factor‑α, offering relief for patients who fail traditional drugs. Biologics often come with a higher price tag, yet their precision reduces broader immune suppression, leading to fewer infections.
For milder cases or as adjuncts, NSAIDs, non‑steroidal anti‑inflammatory eye drops that inhibit cyclooxygenase enzymes can ease discomfort and limit swelling. They’re especially handy after eye surgery or for patients who need a steroid‑sparing bridge. While generally safe, they can irritate the ocular surface if overused.
How These Options Fit Together
The treatment puzzle follows a simple logic: ocular inflammation treatment includes corticosteroids for rapid control, immunosuppressants for long‑term modulation, biologics for targeted precision, and NSAIDs for supportive relief. A doctor may start with steroids, add NSAIDs to smooth the transition, and introduce an immunosuppressant or biologic if the disease proves stubborn. This stepwise approach balances effectiveness with safety, aiming to preserve vision while minimizing drug‑related risks.
Choosing the right regimen also depends on the specific condition. Anterior uveitis often responds well to topical steroids, whereas posterior segment involvement may need systemic immunosuppressants or biologics. Infectious causes demand antibiotics first, with anti‑inflammatory therapy added only once the infection is under control. Understanding the disease pattern helps clinicians pick the most appropriate therapy.
Monitoring is a crucial companion to any plan. Intra‑ocular pressure checks, retinal imaging, and blood work guide dosage adjustments and catch side effects early. Patients who stay engaged—reporting new symptoms, adhering to eye‑drop schedules, and attending follow‑up visits—tend to achieve better outcomes.
Below, you’ll find a collection of articles that dive deeper into each drug class, compare options, and offer practical tips for managing side effects, dosing, and cost. Whether you’re just starting to learn about eye inflammation or you’re looking for the latest evidence on biologic therapy, the posts ahead give actionable insights you can apply right away.
How Steroids Manage Post‑Surgical Eye Inflammation - Complete Guide
Learn how steroids control eye inflammation after surgery, which drugs to use, proper dosing, side‑effects, monitoring, and safe alternatives in a clear, step‑by‑step guide.
About
Medications
Latest Posts

Alpine Lady's Mantle Supplement: Benefits, Uses & Safety Guide
By Marcel Kornblum Sep 22, 2025
Semaglutide: A Promising Treatment for Fatty Liver Disease and More
By Marcel Kornblum Aug 17, 2024
Antiretroviral HIV Medications: Understanding Complex Interactions and Drug Resistance
By Marcel Kornblum Dec 20, 2025

