Personalized Medicine: Tailored Treatments Based on Your Genetics and Lifestyle
When we talk about personalized medicine, a healthcare approach that customizes treatment based on an individual’s genetic makeup, lifestyle, and environment. Also known as precision medicine, it moves away from the one-size-fits-all model and asks: What works for you? This isn’t science fiction—it’s happening right now in clinics, pharmacies, and research labs. For example, if you’re on an antiseizure drug like lamotrigine, your genes might tell your doctor whether a generic version could trigger a seizure—or if you need the brand name to stay stable. That’s pharmacogenomics in action: using your DNA to predict how you’ll respond to a drug.
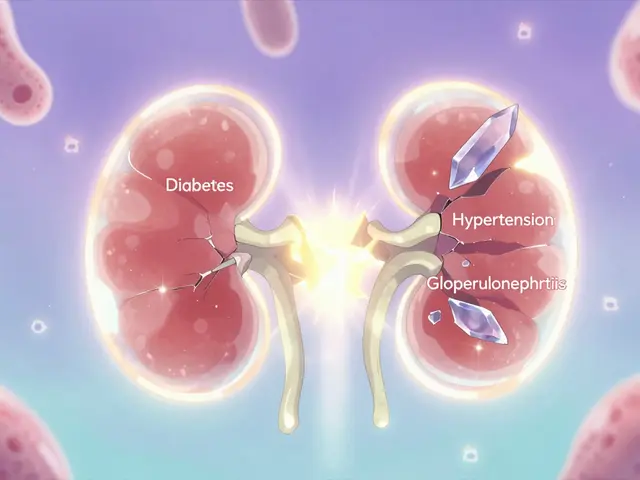
Personalized medicine isn’t just about genes. It also looks at your race, diet, and even your gut health. Studies show that race and ethnicity, factors influencing cancer risk, diagnosis timing, and access to care play a real role in how medications work. A drug that helps one group might not work as well for another due to genetic differences or systemic barriers. Then there’s pharmacogenomics, the study of how genes affect drug metabolism and response. It’s why some people get dizzy on a standard dose of atomoxetine while others need twice as much to feel the effect. Even inactive ingredients, the fillers and binders in pills that aren’t meant to treat anything can make a difference—some people react to dyes or gluten in meds, and personalized medicine helps spot those triggers before they cause harm.
What does this mean for you? It means your treatment doesn’t have to be a guessing game. If you have high blood pressure, your doctor might check if acetyl-L-carnitine could help based on your metabolism. If you’re managing heart failure and have HIV, sacubitril might be a better fit than older drugs. If you’re using eflornithine for ingrown hairs or darifenacin for overactive bladder, personalized medicine helps match the right dose and form—cream vs. gel, tablet vs. capsule—to your body’s needs. It’s not about more drugs. It’s about the right drug, for the right person, at the right time.
Below, you’ll find real-world examples of how this approach is already making a difference—for people with epilepsy, heart conditions, skin issues, and more. These aren’t theoretical ideas. They’re stories of better outcomes, fewer side effects, and smarter choices.
Preventing Adverse Drug Reactions with Pharmacogenetic Testing
Pharmacogenetic testing uses your DNA to predict how you'll react to medications, preventing dangerous side effects. Studies show it cuts adverse drug reactions by 30%, making treatment safer and more effective.
About
Medications
Latest Posts


Jet Lag and Time-Released Medication Dosing Across Time Zones: What Actually Works
By Marcel Kornblum Dec 1, 2025

Strabismus Explained: Understanding Eye Misalignment and Surgical Options
By Marcel Kornblum Feb 5, 2026

Garlic Supplements and Anticoagulants: What You Need to Know About Bleeding Risk
By Marcel Kornblum Jan 4, 2026