Toxic Epidermal Necrolysis (TEN): what it is and why it matters
TEN is a rare but life-threatening reaction that peels large areas of your skin and affects mucous membranes (mouth, eyes, genitals). It usually follows a new medication started days to weeks earlier. If you see fast-spreading blisters, skin coming off in sheets, or painful mucosal sores with fever, treat it as an emergency.
Common causes and who’s at higher risk
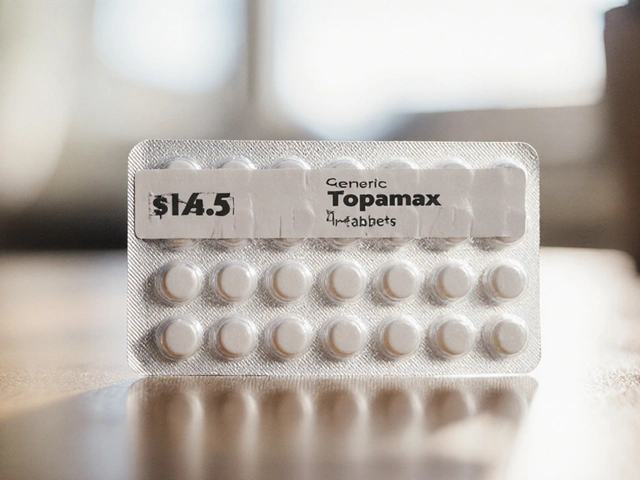
Most cases are triggered by drugs. The usual suspects: sulfa antibiotics like Bactrim (sulfamethoxazole/trimethoprim), allopurinol, several anticonvulsant drugs (carbamazepine, lamotrigine, oxcarbazepine), some NSAIDs (oxicam class), and certain antibiotics. Infections can sometimes trigger similar reactions, but drug exposure is the main alarm bell. Genetic markers also raise risk—HLA-B*1502 is linked to carbamazepine reactions in some Asian populations, and HLA-B*5801 increases risk with allopurinol.
Risk is highest in the first 1–8 weeks after starting a new medicine. That means pay attention when your doctor prescribes something new and watch for early symptoms.
How to spot TEN quickly and what to do right away
Warning signs to watch for: fever plus a spreading red or purplish rash, painful blisters, skin that peels when touched, raw mouth or eye sores, trouble breathing or swallowing. If any of those appear, stop the suspected drug immediately and get to the emergency room. Tell staff every medicine you recently took, even over-the-counter drugs and supplements. Photos of how the rash started can help clinicians.
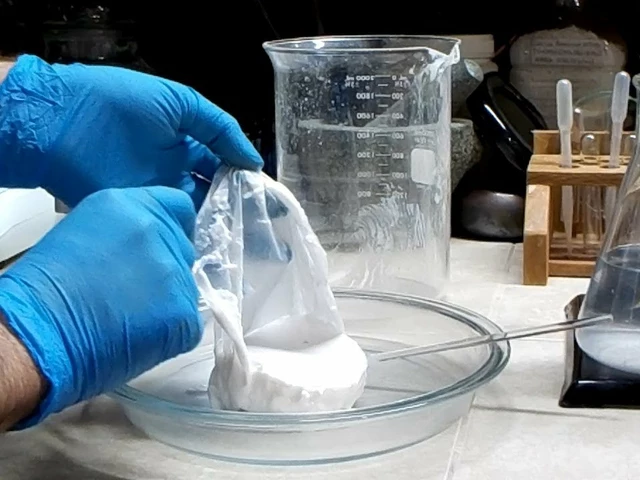
Treatment happens in hospital—often in an ICU or burn unit. The big priorities are: stop the offending drug, support fluids and electrolytes, manage pain, prevent infection, and protect eyes and mucous membranes. Wound care looks a lot like burn care. Specialists (dermatology, ophthalmology, intensive care) coordinate treatment. Some centers use drugs like IVIG, cyclosporine, or short steroid courses; evidence varies, so specialists decide case by case.
Don’t try creams, home remedies, or oral steroids on your own. Re-exposure to the culprit drug can cause a worse reaction or be fatal. Make sure any drug that likely caused TEN is clearly documented in your chart and your pharmacy records.
Want to prevent problems? Ask your prescriber about alternatives if you have known genetic risks, and mention any past unusual drug reactions. Watch closely during the first two months after starting new meds. If you’re searching for more on specific drugs linked to TEN, our site has practical guides on Bactrim, oxcarbazepine, common antibiotics, and safer alternatives.
Fast recognition and stopping the culprit drug save lives. If you’re worried about a new rash or symptoms after starting a medicine, don’t wait—seek emergency care and tell clinicians exactly which drugs you’ve taken.
The Alarming Link Between Diflucan and Severe Skin Disorders: A Comprehensive Lawsuit Update
A recent update on lawsuits has put a spotlight on Diflucan, a popular antifungal medication, for its possible connection to severe skin conditions, Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN). Legal firm, Schmidt & Clark, LLP, is pursuing cases nationwide, offering insights into the drug's adverse effects and the legal recourse for affected individuals.
About
Health and Wellness
Latest Posts

Aluminium Hydroxide in Food: Is it Safe?
By Marcel Kornblum Jun 18, 2023

Inactive Ingredient Differences: Can Excipients Affect Safety or Efficacy?
By Marcel Kornblum Nov 12, 2025

How to Create a Medication Expiration Review Schedule
By Marcel Kornblum Dec 3, 2025