Treatment Combination: How to Combine Medications Safely
Using two or more drugs together can be smart or risky. Combination therapy can control stubborn infections, treat chronic conditions, or reduce side effects by lowering each drug's dose. But mixing meds also raises the chance of interactions, extra side effects, and unexpected lab changes. This page helps you spot when combinations make sense and how to avoid common dangers.
When combinations help
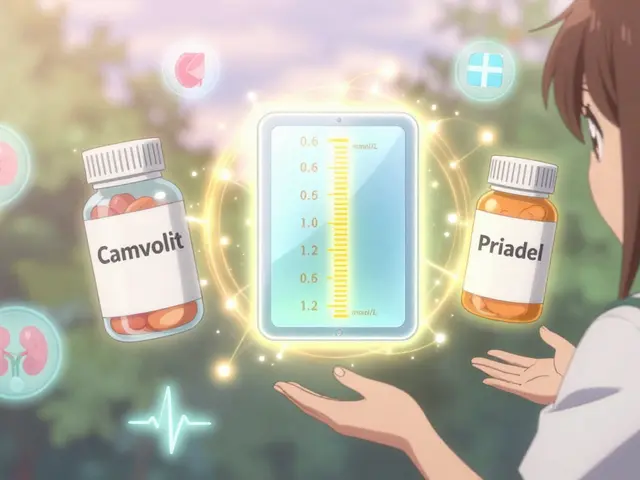
Think of combinations as teamwork: one drug fills a gap the other leaves. For infections, a doctor may pair antibiotics to cover different bacteria or prevent resistance—however, choices matter. For example, if amoxicillin isn't working, a clinician might switch to an effective alternative or combine agents carefully rather than stacking similar drugs. In chronic disease, combining drugs with different actions—like a blood sugar drug plus a GLP-1 agent such as semaglutide for fatty liver and weight control—can improve outcomes more than either alone.
In mental health, switching or pairing antidepressants requires thought. Some people use Wellbutrin (bupropion) alongside an SSRI to boost effect or reduce sexual side effects, but every pairing should be guided by a prescriber to avoid serotonin overload or seizure risk. For pain, combining drugs (for example, a nerve pain agent plus an SNRI) can help when a single drug falls short.
How to stay safe
Start by making a full list of everything you take: prescriptions, OTC meds, supplements, and herbs. Show it to every clinician and your pharmacist. Ask these simple questions: Why do I need this drug? What benefit should I expect? What side effects should I watch for? Could this interact with my other meds?
Watch for these red flags: drugs that raise the same lab risk (like liver stress), medicines that both lengthen the QT interval (some antibiotics such as azithromycin and certain antidepressants like citalopram), and combinations that increase serotonin (multiple SSRIs, SNRIs, triptans) which can trigger serotonin syndrome. Another real example: Bactrim (sulfamethoxazole/trimethoprim) can raise warfarin levels and cause bleeding—so your INR needs checking if both are used.
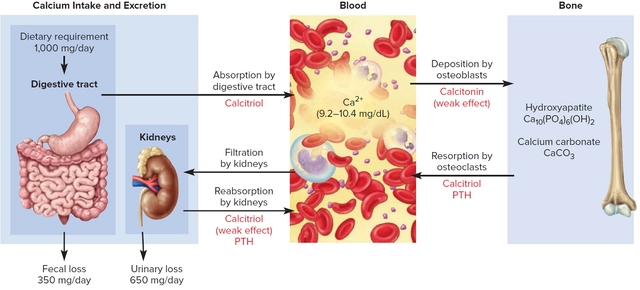
Ask about dose adjustments and monitoring. Some combinations need blood tests, ECGs, or checking sodium or liver levels. If a new symptom appears after adding a drug—dizziness, fast heart rate, confusion, severe rash—contact your provider immediately.
Finally, don’t stop or start meds on your own. If you think a drug isn’t working or causes side effects, bring specifics to your prescriber—what changed, when, and how severe. That makes it easier to decide whether to switch, stop, or safely add another medicine.
Combining treatments can improve care, but only when chosen and monitored carefully. Use your pharmacist and doctor as a team, keep an up-to-date meds list, and speak up about side effects. That’s how you get the benefits without the surprises.
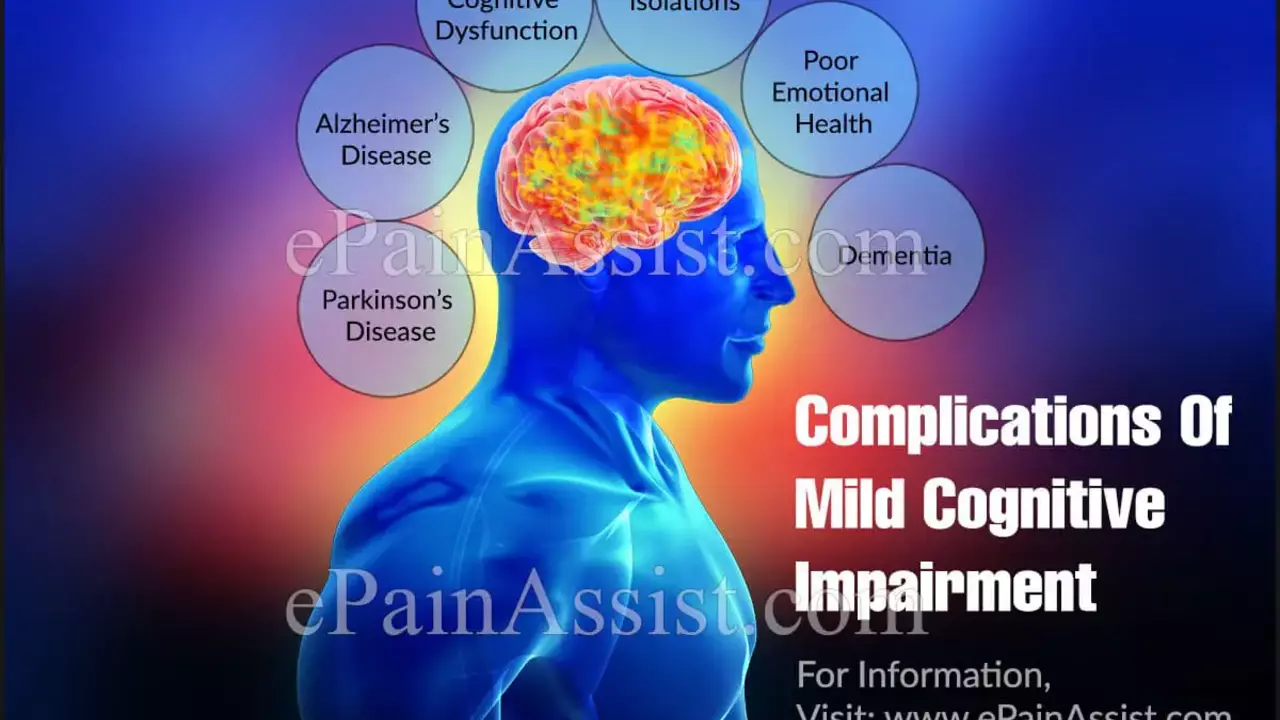
Rivastigmine and Cognitive Training: A Winning Combination for Alzheimer's Disease?
In my latest exploration, I've delved into the promising potential combination of Rivastigmine and cognitive training for Alzheimer's disease. It appears that Rivastigmine, a drug traditionally used to alleviate Alzheimer's symptoms, may have its effectiveness significantly enhanced when paired with cognitive training. This training focuses on boosting the mental capabilities of patients, thereby potentially slowing the disease's progression. While more research is needed, the initial results are exciting and bring a ray of hope for those battling this devastating disease. It's truly fascinating how combining different strategies could potentially change the game in Alzheimer's treatment.
About
Health and Medicine
Latest Posts
Understanding the side effects and risks of calcitonin therapy
By Marcel Kornblum May 29, 2023

Arimidex (Anastrozole) vs Other Aromatase Inhibitors: A Practical Comparison
By Marcel Kornblum Oct 2, 2025

Tympanites Explained: Causes, Symptoms & Treatment
By Marcel Kornblum Oct 11, 2025