When someone starts forgetting where they put their keys-again-it’s easy to brush it off as aging. But when those lapses turn into forgetting a child’s name, getting lost in their own neighborhood, or repeating the same question every five minutes, it’s no longer just forgetfulness. It’s Alzheimer’s disease. And it doesn’t just affect the person diagnosed. It reshapes the lives of everyone around them.
What Alzheimer’s Does to Memory
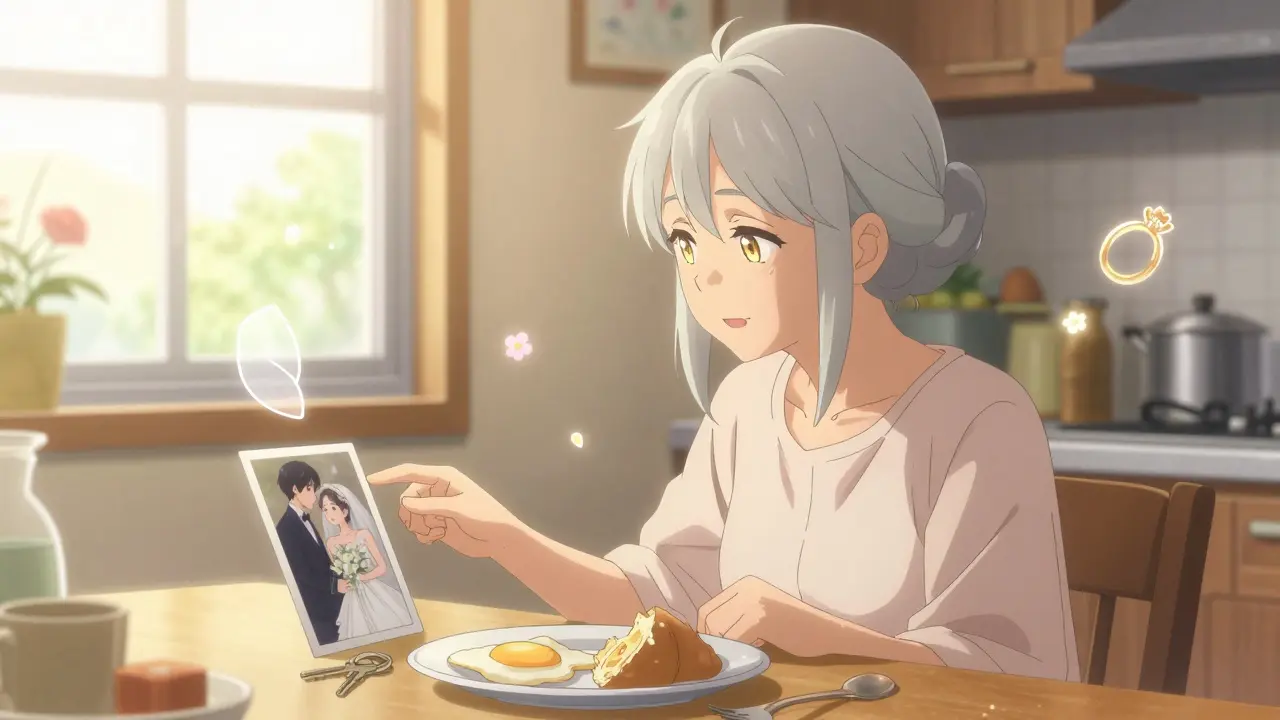
Alzheimer’s doesn’t just make you forget things. It erases the ability to form new memories in the first place. The brain’s hippocampus, the area responsible for storing recent experiences, is one of the first places damaged. That’s why someone with early-stage Alzheimer’s might remember their wedding day clearly but can’t recall what they had for breakfast. This isn’t like normal forgetfulness. Normal forgetfulness? You walk into a room and forget why. Alzheimer’s? You walk into a room and don’t recognize it as your own. You might look at your spouse and not know who they are. You might ask the same question over and over because your brain can’t hold onto the answer. Studies show that in the earliest stages, people struggle most with episodic memory-the memory of events and experiences. They forget conversations, misplace items, repeat stories, and have trouble learning new routines. Formal testing reveals they don’t just forget words or names-they can’t learn them in the first place. Even when given clues, their brains struggle to retrieve what’s been lost. As the disease moves into later stages, long-term memories start to fade too. People forget their own life stories. They may not remember their children’s names, their past jobs, or even their own birth year. By the final stage, they may no longer recognize themselves in the mirror.The Five Stages of Alzheimer’s
Alzheimer’s doesn’t happen overnight. It unfolds slowly, often over a decade or more. While every person’s journey is different, most follow a general pattern divided into five stages by experts at the Mayo Clinic.- Preclinical Alzheimer’s - This stage happens years before any symptoms appear. Brain changes are already underway-amyloid plaques and tau tangles are building up-but the person shows no signs of memory loss. This is only detectable through brain scans or spinal fluid tests, not yet used in routine care.
- Mild Cognitive Impairment (MCI) - This is where families start noticing something’s off. The person forgets recent events, struggles with planning, loses track of conversations, and may get lost in familiar places. They still drive, cook, and manage money-but they need help with complex tasks. Many people in this stage worry they have dementia. They’re right to be concerned: about 8 out of 10 people with MCI due to Alzheimer’s will develop full dementia within six years.
- Mild Dementia - Memory loss becomes obvious to everyone. The person repeats questions, forgets appointments, gets confused about the day or season, and may have trouble finding the right words. They might misplace things and accuse others of stealing. Mood changes like anxiety, irritability, or depression are common. At this point, they still live independently but need help with bills, medications, and meal planning.
- Moderate Dementia - This is the longest and often most challenging stage. The person needs help with daily tasks: choosing clothes, bathing, using the toilet. They may wander, become suspicious of loved ones, or believe they’re being followed. Sleep is disrupted. They might not recognize family members anymore. Incontinence begins. Caregivers report this stage is emotionally exhausting-repetitive questions, accusations, and nighttime wandering can break even the most patient person.
- Severe Dementia - The person loses the ability to communicate. They may stop speaking entirely or only make sounds. They can’t walk without help, sit up without support, or swallow safely. They become bedbound. They don’t respond to names or faces. They may smile when touched or hum along to music, but they no longer understand what’s happening around them. This is when full-time care becomes non-negotiable.
Why Caregivers Are the Real Frontline
No drug can cure Alzheimer’s. No treatment can stop it. The only real defense is care-and that care almost always comes from family. In 2023, over 11 million Americans provided unpaid care for someone with Alzheimer’s or another dementia. They spent an average of 27 hours a week doing it. That’s more than a full-time job. And it’s not just time-it’s emotional labor. Thirty percent of caregivers say they’re physically worn down. Nearly 40% say their stress level is high or very high. Caregivers aren’t just helping with baths and meals. They’re managing delusions (“My daughter stole my purse”), preventing wandering (installing door alarms, hiding car keys), dealing with aggression, and holding back tears when their loved one doesn’t recognize them anymore. One caregiver in Adelaide told me: “I used to argue with my husband when he said his mother was in the kitchen. He’d get angry if I said she was dead. Now I just say, ‘Yes, she’s making tea. Want some?’ It’s not lying. It’s keeping him calm.” That’s validation therapy-a simple but powerful technique. Instead of correcting someone with dementia, you meet them where they are. If they think they’re at work, talk about their job. If they’re looking for their dead spouse, sit with them and say, “I know you miss her.”
What Care Looks Like at Each Stage
Early Stage: Focus on independence. Use calendars, reminder apps, labeled cabinets, and pill organizers. Encourage routines-same breakfast time, same walk route. Keep them socially active. Don’t take away the car too soon. Drive with them first, then suggest they let someone else handle the shopping. Middle Stage: Safety becomes priority number one. Remove throw rugs. Install grab bars in the bathroom. Lock up sharp objects and cleaning supplies. Use door alarms to prevent wandering. Create a calm environment-reduce noise, keep lighting bright, play familiar music. Use simple, one-step instructions: “Let’s wash your hands,” not “Go to the bathroom and wash your hands, dry them, and come back.” Late Stage: Comfort is everything. They may no longer eat solid food-switch to soft, easy-to-swallow meals. Watch for signs of pain-they can’t tell you anymore. A grimace, clenched fists, or restlessness might mean they’re hurting. Keep their skin clean and dry to prevent bedsores. Hold their hand. Sing to them. Play their favorite songs. Even if they don’t respond, their body still feels the warmth.What No One Tells You About Late Stage
Many caregivers expect the final stage to be the hardest emotionally. But many say the opposite. In late-stage Alzheimer’s, the person is no longer aware of their surroundings. There’s no more screaming, no more accusations, no more wandering at 3 a.m. They’re quiet. Still. Often peaceful. One woman on a caregiver forum wrote: “The hardest part was when he knew what was happening. The last six months, he didn’t know me anymore. But he’d smile when I held his hand. That was enough.” That’s the cruel twist of Alzheimer’s: the person you loved is gone before the body is. But the love? It doesn’t disappear. It just changes shape.
Help Is Out There-If You Know Where to Look
You don’t have to do this alone. Medicare covers up to five days of respite care per year for caregivers of hospice-eligible patients. Local Area Agencies on Aging offer free caregiver training, support groups, and home visits. Organizations like Dementia Australia and the Alzheimer’s Association provide 24/7 helplines and online forums. There are apps now that track wandering, remind patients to take meds, and even detect falls. Some communities have “dementia-friendly” stores where staff are trained to help confused customers. There are even memory cafes-quiet places where people with dementia and their caregivers can sit, sip tea, and talk without judgment. The biggest mistake caregivers make? Waiting until they’re broken to ask for help. Don’t wait. Reach out now. Even if it’s just one hour a week of someone sitting with your loved one so you can shower or sleep.What’s Changing in Alzheimer’s Treatment
For decades, the only drugs available were donepezil and memantine-medications that slightly slow memory loss but don’t change the course of the disease. That changed in 2023 when the FDA approved lecanemab, the first drug shown to slow cognitive decline by targeting amyloid plaques in the brain. It’s not a cure. It doesn’t bring back memories. But in clinical trials, it reduced decline by 27% over 18 months. It requires monthly IV infusions and regular brain scans to check for dangerous swelling. It’s only for people in the early stages. And it costs over $25,000 a year. Still, it’s a sign that science is finally catching up. Blood tests to detect Alzheimer’s before symptoms appear are coming. By 2028, a simple finger-prick test could tell you if you’re at risk-years before memory loss starts. But here’s the hard truth: these advances won’t help most people. The tests cost thousands. The drugs are expensive. They’re not available in most countries. And they won’t help someone who’s already in the middle or late stage. That’s why care still matters more than ever.Final Thought: You Are Not Failing
If you’re caring for someone with Alzheimer’s, you’re doing something almost no one else can do. You’re holding space for someone who’s slipping away. You’re showing up on the days you’re exhausted. You’re smiling when they don’t know your name. You’re loving them even when they don’t remember how to love back. That’s not failure. That’s courage. You don’t need to be perfect. You don’t need to know all the answers. You just need to be there. And that’s enough.What are the first signs of Alzheimer’s disease?
The earliest signs include forgetting recent conversations or events, repeating questions, misplacing items in odd places, having trouble finding the right words, and showing poor judgment-like giving away large sums of money or neglecting personal hygiene. These aren’t normal aging slips. They’re persistent, worsening, and interfere with daily life.
Can Alzheimer’s be reversed or cured?
No, Alzheimer’s cannot be reversed or cured yet. Current treatments like donepezil and memantine may temporarily ease symptoms, and newer drugs like lecanemab can slow decline in early stages by targeting brain plaques. But none stop the disease from progressing. Care, not cure, remains the most effective approach.
How long do people live after an Alzheimer’s diagnosis?
Life expectancy after diagnosis varies widely. Some people live 4 to 8 years, while others survive 20 years or more. The average is about 8 to 10 years. Factors like age at diagnosis, overall health, and access to care play a big role. Most people don’t die directly from Alzheimer’s-they die from complications like pneumonia, infections, or falls.
What’s the difference between Alzheimer’s and other types of dementia?
Alzheimer’s is the most common type, accounting for 60-80% of dementia cases. It starts with memory loss, especially recent memories. Other dementias, like Frontotemporal Dementia, often begin with personality changes or language problems before memory is affected. Vascular dementia follows strokes and comes on more suddenly. Only a medical evaluation can tell the difference.
How can I help a caregiver of someone with Alzheimer’s?
Offer specific help, not just “Let me know if you need anything.” Say: “I’ll come Tuesday to sit with them so you can nap,” or “I’ll pick up groceries this week.” Listen without trying to fix things. Send a meal. Share a funny memory of the person. Caregivers need to feel seen, not pitied. Respite care and support groups are lifelines-help them find one.
When should I consider professional care or a memory facility?
Consider professional care when safety is at risk-wandering, falling, forgetting to eat or take meds, or when the caregiver is physically or emotionally overwhelmed. If you’re losing sleep, getting sick, or feeling hopeless, it’s not weakness to ask for help. Memory care units offer trained staff, secure environments, and structured routines that families can’t always provide at home.





John O'Brien
January 28, 2026 at 05:23
I've been caring for my mom for 5 years now. The worst part? She still smiles when I sing her favorite songs. Doesn't know who I am, but she knows the melody. That's all that matters now.
And yeah, I've argued with her about her dead mom too. Now I just say 'yeah, she's making pancakes.' She calms right down. No need to ruin her day with truth.