Acne & Skin Infection Antibiotic Selector
Select Your Condition
Medical History
Recommended Treatment
When acne or a skin infection stubbornly refuses to clear up, many turn to oral antibiotics. Cleocin is a brand name for clindamycin, a lincosamide antibiotic used to treat bacterial skin infections and acne vulgaris. But is it always the best choice? This guide walks you through the most common alternatives, the factors to weigh, and who should pick which option.
TL;DR
- Cleocin works well for acne and some skin infections but can cause resistance if overused.
- Doxycycline and minocycline are first‑line oral acne drugs with anti‑inflammatory benefits.
- Erythromycin and azithromycin are useful for people who can’t tolerate lincosamides.
- Topical benzoyl peroxide, retinoids, or salicylic acid are non‑antibiotic alternatives that avoid resistance.
- Choose based on infection type, side‑effect profile, pregnancy safety, and cost.
How to Pick the Right Antibiotic
Before diving into the drug‑by‑drug rundown, think about these decision points. They apply whether you’re a patient, a dermatologist, or a primary‑care provider.
- Target condition: Is it acne, cellulitis, impetigo, or another skin infection?
- Resistance risk: Has the patient used antibiotics recently?
- Side‑effect tolerance: Gastrointestinal upset, photosensitivity, or yeast overgrowth?
- Pregnancy or breastfeeding: Not all antibiotics are safe.
- Cost and insurance coverage: Some generics are cheap, others require prior authorization.
Keeping these factors in mind will help you decide whether Cleocin is the right fit or if another option suits better.
Cleocin (Clindamycin)
Clindamycin belongs to the lincosamide class. It blocks bacterial protein synthesis by binding to the 50S ribosomal subunit. Typical oral dose for acne: 300mg twice daily for 12weeks. For skin infections, the dose can range from 150‑450mg three times daily.
Pros:
- Effective against Staphylococcus aureus (including some MRSA strains) and Propionibacterium acnes.
- Often well‑tolerated; low risk of photosensitivity.
- Can be combined with topical benzoyl peroxide to reduce resistance.
Cons:
- Higher chance of causing Clostridioides difficile infection.
- Resistance can develop quickly if used for more than three months.
- Not recommended during pregnancy (Category B).
Alternative #1: Doxycycline
When you first see Doxycycline is a tetracycline‑class antibiotic that also has strong anti‑inflammatory properties. The standard acne dose is 100mg once or twice daily for 12‑16weeks.
Pros:
- Excellent for inflammatory acne.
- Lower risk of severe GI complications compared with clindamycin.
- Can be used in combination with topical retinoids.
Cons:
- Photosensitivity is common; sunscreen is a must.
- May cause esophageal irritation if not taken with water.
- Contraindicated in pregnancy (Category D).
Alternative #2: Minocycline
Minocycline is another tetracycline derivative that penetrates skin well. Typical dosing for acne is 100mg once daily.
Pros:
- Potent anti‑bacterial and anti‑inflammatory effects.
- Longer half‑life allows once‑daily dosing.
- Often effective when doxycycline fails.
Cons:
- Higher chance of vestibular side‑effects (dizziness, vertigo).
- Can cause hyperpigmentation of skin and nail beds.
- Also not safe in pregnancy.
Alternative #3: Erythromycin
Erythromycin is a macrolide that works by inhibiting bacterial protein synthesis. Dose for acne ranges from 250‑500mg four times daily.
Pros:
- Useful for patients allergic to tetracyclines.
- Has a relatively favorable safety profile for short courses.
Cons:
- Gastrointestinal upset is common; needs to be taken with food.
- Resistance rates have risen in recent years.
- Can cause hepatotoxicity at high doses.
Alternative #4: Azithromycin
Azithromycin is a macrolide with a long half‑life, allowing short‑course therapy. A common acne regimen is 500mg once daily for three days, then twice weekly.
Pros:
- Convenient dosing schedule improves adherence.
- Lower GI side‑effects compared with erythromycin.
Cons:
- Higher cost than generic tetracyclines.
- Potential QT‑interval prolongation; caution with cardiac patients.

Non‑Antibiotic Alternatives
Antibiotics are not the only way to tackle acne or skin infections. Here are two popular non‑antibiotic options that can be used alone or alongside oral drugs.
Topical Benzoyl Peroxide
Benzoyl peroxide is a keratolytic that kills bacteria by oxidizing bacterial proteins. Concentrations range from 2.5‑10% in gels or creams.
Benefits include rapid reduction of P. acnes colonies and minimal risk of systemic side‑effects. It also helps prevent antibiotic resistance when combined with oral agents.
Retinoids (Tretinoin, Adapalene)
Topical retinoids promote cell turnover, unclog pores, and reduce inflammation. They are especially effective for comedonal acne.
When used correctly, retinoids can lessen the need for long‑term antibiotics.
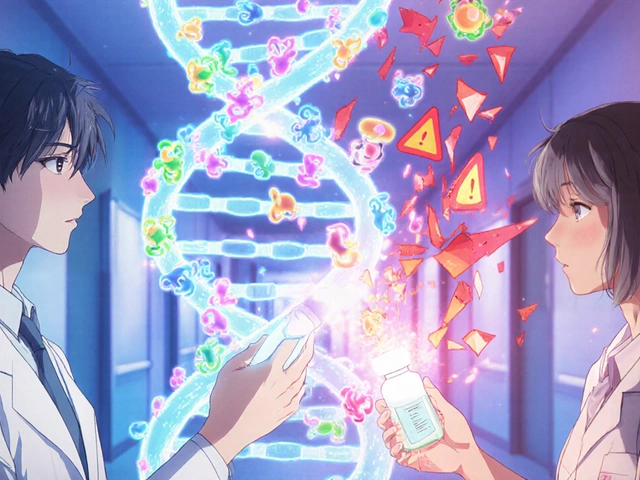
Side‑By‑Side Comparison Table
| Antibiotic | Typical Acne Dose | Major Advantage | Top Concern | Pregnancy Safety |
|---|---|---|---|---|
| Clindamycin (Cleocin) | 300mg BID | Effective against MRSA strains | C. difficile infection risk | Category B (caution) |
| Doxycycline | 100mg BID | Strong anti‑inflammatory effect | Photosensitivity | Category D (avoid) |
| Minocycline | 100mg QD | Once‑daily dosing | Dizziness, hyperpigmentation | Category D (avoid) |
| Erythromycin | 250‑500mg QID | Alternative for tetracycline allergy | GI upset, resistance | Category B |
| Azithromycin | 500mg QD3days then 2×/week | Convenient short courses | Cost, QT risk | Category B |
When to Stick with Cleocin
If your dermatologist has confirmed that the infection involves MRSA or if you have a long‑standing acne flare that hasn’t responded to tetracyclines, Cleocin can be a smart pick. Pairing it with a topical benzoyl peroxide reduces the chance of resistance, especially after the first month.
When to Switch to an Alternative
Consider moving away from Cleocin if any of the following apply:
- History of recent C. difficile infection.
- Pregnancy or planning to become pregnant.
- Developing severe GI upset or rash.
- Need for a more convenient dosing schedule.
In those cases, doxycycline or a short course of azithromycin often delivers comparable acne control with fewer systemic risks.
Practical Tips for Patients
- Take oral antibiotics with a full glass of water; stay upright for 30minutes to avoid esophageal irritation.
- Use a gentle cleanser and non‑comedogenic moisturizer to limit skin dryness.
- Never skip the topical benzoyl peroxide unless you’re allergic - it cuts resistance odds dramatically.
- Set a reminder to stop the antibiotic after the prescribed period; prolonged use fuels resistance.
- Report any persistent diarrhea or severe abdominal pain to your doctor immediately.
Cost and Access Overview (2025)
Generic clindamycin caps are typically $0.30 per tablet, while brand‑name Cleocin can be $2‑3 per tablet. Doxycycline generic runs about $0.15 per tablet, making it the most budget‑friendly option for long‑term acne therapy. Azithromycin, especially the extended‑release brand, can reach $1 per tablet. Insurance plans usually cover generics but may require prior authorization for brand names.
Key Takeaways
- Cleocin is a potent antibiotic, especially against resistant staph, but carries a higher C. difficile risk.
- Tetracyclines (doxycycline, minocycline) are first‑line for inflammatory acne with anti‑inflammatory benefits.
- Macrolides (erythromycin, azithromycin) serve as alternatives when tetracycline use is contraindicated.
- Non‑antibiotic topicals like benzoyl peroxide and retinoids can cut the duration of oral therapy.
- Always balance efficacy, side‑effects, pregnancy safety, and cost before committing to a regimen.

Frequently Asked Questions
Can I use Cleocin and benzoyl peroxide together?
Yes. Combining oral clindamycin with a topical benzoyl peroxide gel (2.5‑5%) reduces bacterial resistance and often speeds up acne clearance.
How long should I stay on Cleocin for acne?
Most dermatologists limit oral clindamycin to 3‑4months. Extending beyond that raises the chance of C. difficile infection and resistance.
Is clindamycin safe during pregnancy?
Clindamycin is classified as Pregnancy Category B, meaning animal studies show no risk but there are limited human data. Discuss with your OB‑GYN before starting.
What are signs of C. difficile infection?
Watch for persistent watery diarrhea, abdominal cramping, and fever. If any appear while on clindamycin, seek medical care promptly.
Are there over‑the‑counter alternatives to antibiotics for acne?
Yes. Products containing benzoyl peroxide, salicylic acid, or over‑the‑counter retinoids (e.g., adapalene 0.1%) can control mild‑to‑moderate acne without prescription antibiotics.
Which antibiotic works best for fast‑growing skin infections?
For acute cellulitis or impetigo, clindamycin or a beta‑lactam like cephalexin are common first choices. The exact drug depends on culture results and allergy history.


Brian Skehan
September 29, 2025 at 18:09
Look, the whole clindamycin hype is just another pharma cash grab. They love to shove broad‑spectrum pills on anyone who walks into a dermatologist’s office, hoping we’ll swallow the resistance bullet with it. If you actually read the side‑effect warnings, you’ll see the C. difficile nightmare they hide in the fine print. And don’t even get me started on the “MRSA‑friendly” marketing spin – that’s a textbook case of fear‑mongering.