Brand Drug Strategy: How Companies Control Prices, Access, and Patient Choices
When you hear brand drug strategy, the plan pharmaceutical companies use to protect profits, delay generics, and control how doctors and patients use their medicines. Also known as pharmaceutical market strategy, it’s not just about advertising—it’s about locking in customers, extending monopolies, and shaping what’s affordable. This isn’t theoretical. It’s why your $500 pill has a $20 generic version sitting right next to it, and why your insurance won’t cover the brand unless you try the cheap one first.
Behind every drug patent, a legal monopoly that lets a company sell a medicine without competition for 20 years. Also known as patent protection, it’s the foundation of brand drug strategy. But companies don’t just wait for the clock to run out. They file new patents on tiny changes—like a different pill shape, a new time-release formula, or a slightly altered chemical combo—to reset the clock. This trick, called evergreening, keeps generics off shelves for years longer than most people realize. Meanwhile, generic substitution, when pharmacies swap a brand-name drug for its cheaper copy unless the doctor says no. Also known as generic switching, it’s the main way patients save money—but brand drug strategy works hard to block it. Some companies pay generic makers to delay release. Others flood pharmacies with free samples so doctors never switch. And if you’re on a chronic med like a statin or antiseizure drug, even small differences in inactive ingredients can trigger side effects, making doctors hesitant to switch—something we see in posts about antiseizure medications and inactive ingredients.
It’s not just about money. pharmaceutical pricing, how drug makers set what you pay, often with no connection to how much it cost to make. Also known as drug cost models, it’s the engine behind brand drug strategy. A pill that costs pennies to produce can be priced at hundreds because the company claims it’s "innovative" or "specialized." That’s why you’ll see articles comparing Actigall vs alternatives or Zyvox vs alternatives—patients are forced to ask if the brand is worth the cost, or if the generic works just as well. Even when generics exist, Pharmacy Benefit Managers (PBMs) and insurers often structure formularies to favor the brand through rebates and hidden fees, a system we break down in posts about generic drug prices and PBM negotiations.
What does this mean for you? If you’re on a long-term medication, you’re likely caught in the middle of a financial game you didn’t sign up for. Brand drug strategy isn’t about better outcomes—it’s about controlling access. That’s why the posts here cover everything from how genetic testing can help you avoid bad reactions to why support groups improve adherence. Because when you understand how the system works, you can ask the right questions: Is this the only option? Why is the generic cheaper? Did my doctor know about the cost difference? The answers aren’t always easy, but they’re out there—and you’ll find them below.
Authorized Generics: How Brand Drug Companies Respond to Patent Expiration
Authorized generics are brand-name drugs sold under a different label after patent expiration. They're identical to the original, lower in price, and used by manufacturers to compete with generics. Here's how they work and why they matter.
About
Medications
Latest Posts


8 Alternatives to Wellbutrin Sr
By Marcel Kornblum Feb 28, 2025

How Support Groups and Community Programs Improve Medication Compliance
By Marcel Kornblum Nov 26, 2025
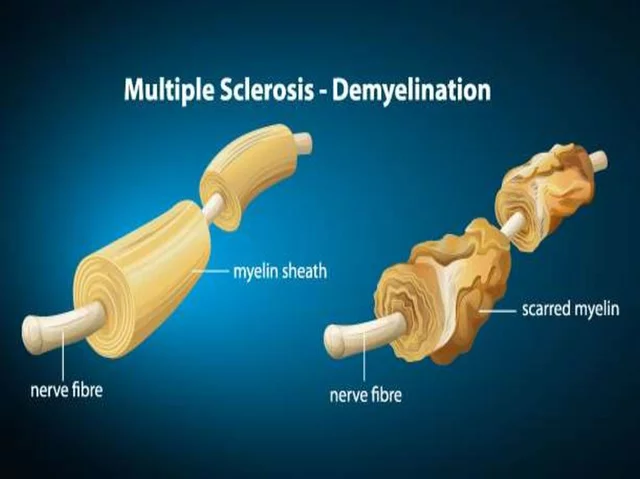
The potential use of dipyridamole in the treatment of multiple sclerosis
By Marcel Kornblum May 6, 2023

