Generic vs Brand Name Medications: What Really Matters
When you pick up a prescription, you might see two options: a generic medication, a drug that contains the same active ingredient as a brand-name version but is sold under its chemical name. Also known as non-brand drugs, these are often cheaper and just as effective. Or you might get the brand name drug, the original version developed by a pharmaceutical company and sold under a trademarked name. The big question isn’t just cost—it’s whether the difference between them actually affects how you feel or if you’re just paying more for a logo.
Here’s the truth: by law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand version. That means if you’re taking generic lisinopril or generic metformin, your body gets the same medicine that works the same way. But here’s where things get messy: the inactive ingredients, the fillers, dyes, and binders that hold the pill together or help it dissolve can vary. These excipients don’t treat your condition, but they can change how fast the drug gets into your system, trigger allergies, or cause stomach upset in sensitive people. That’s why some folks swear their brand-name adapalene works better than the generic, or why switching from Zyvox to linezolid made them feel off—even though both have the same active component.
It’s not just about pills either. The same logic applies to antifungal treatments, like Fulvicin versus terbinafine, or immunosuppressants, like cyclosporine versus tacrolimus. Even when the active ingredient matches, differences in manufacturing, coating, or release timing can make a real difference in how your body responds. For people with chronic conditions—like heart failure on sacubitril, epilepsy on valproate, or ADHD on atomoxetine—that tiny shift in absorption can mean the difference between control and a bad day.
So what should you do? Don’t assume generics are always interchangeable. If you’ve been stable on a brand drug and your doctor says you can switch, ask about the specific generic being used. If you notice changes in how you feel—more side effects, less effectiveness, or new reactions—talk to your pharmacist. They can check if the manufacturer changed, or if your body just doesn’t respond well to a certain filler. The bottom line: generic drugs are safe, legal, and cost-saving. But your body isn’t a lab test. It’s a person. And sometimes, the difference between two pills isn’t in the active ingredient—it’s in the details you can’t see on the label.
Antiseizure Medications and Generic Substitution: Risks and Best Practices
Generic antiseizure medications can save money, but for NTI drugs like lamotrigine and carbamazepine, even small changes in absorption can trigger seizures. Learn the risks, who’s most vulnerable, and how to protect your treatment.
About
Medications
Latest Posts

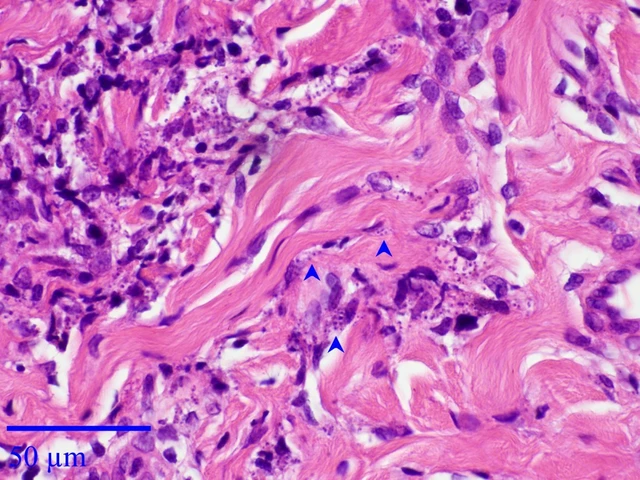
The Use of Fusidic Acid in the Management of Cutaneous Leishmaniasis
By Marcel Kornblum May 21, 2023

Arcalion (Sulbutiamine) vs Top Alternatives - Benefits, Risks & Best Uses
By Marcel Kornblum Oct 21, 2025

Buying Viagra and ED Meds Safely: Honest Review of trysildenafil.com
By Marcel Kornblum Jul 30, 2025

