Medication Efficacy: What Works, Why It Matters, and How to Know for Sure
When you take a pill, you expect it to medication efficacy—to reduce pain, lower blood pressure, stop seizures, or clear up acne. But not all drugs work the same for every person. Even small differences in how your body absorbs or processes a medicine can make the difference between control and crisis. This isn’t theory—it’s why someone on generic lamotrigine might suddenly have a seizure, or why a cheap antibiotic might fail to kill an infection that another one handles easily. Medication efficacy, the measurable ability of a drug to produce the desired therapeutic effect under real-world conditions. Also known as clinical effectiveness, it’s not just about the label on the bottle—it’s about how your body, your diet, your other meds, and even your genetics all play a part.
Think about generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as generic switching, it’s common, affordable, and usually safe—except when it isn’t. For NTI drugs like carbamazepine or levothyroxine, even a 5% change in absorption can throw your whole treatment off. That’s why some people do fine switching, while others end up back in the ER. Then there’s antiseizure medications, drugs designed to prevent or reduce epileptic seizures by stabilizing brain activity. Also known as antiepileptic drugs, they’re one of the clearest examples of how efficacy isn’t just about the active ingredient—it’s about consistency, timing, and what else you’re taking. Evening primrose oil might sound harmless, but it can lower your seizure threshold when mixed with antipsychotics. And if you’re on atomoxetine for ADHD, what you eat for breakfast can boost or wreck its effect. Even antibiotic alternatives, other drugs used to treat infections when first-line options fail or cause side effects. Also known as second-line antibiotics, they’re not just backups—they’re often more effective, faster, or safer for your gut. Zyvox works where others don’t, but only if you avoid certain foods. Terbinafine clears nail fungus faster than Fulvicin, and it doesn’t need months of daily pills. And supplement effects, how over-the-counter vitamins or herbal products interact with prescription drugs or alter their performance. Also known as nutraceutical interactions, they’re rarely talked about—but acetyl-L-carnitine can help your circulation, and sulbutiamine might sharpen your focus, if you know how to use them right.
Medication efficacy isn’t a one-size-fits-all number on a chart. It’s personal. It’s messy. It’s shaped by your liver, your diet, your other prescriptions, your sleep, and even your stress levels. The posts below don’t just list drugs—they show you exactly how and why some work better than others, when to stick with what you’ve got, and when to ask for something different. You’ll find real comparisons: which antifungal actually clears your toenail faster, whether your generic lisinopril is doing the job, how diet changes can make atomoxetine work better, and why switching from Arimidex to letrozole might be the smart move for your breast cancer treatment. No fluff. No marketing. Just what works, what doesn’t, and what you need to ask your doctor next time.
Inactive Ingredient Differences: Can Excipients Affect Safety or Efficacy?
Inactive ingredients in medications-called excipients-may not be as harmless as once thought. New research shows some can affect drug absorption, trigger reactions, or even interact with your body’s biology. Here’s what you need to know.
About
Medications
Latest Posts


Buy Cheap Generic Warfarin Online - Affordable Anticoagulant Guide 2025
By Marcel Kornblum Oct 1, 2025
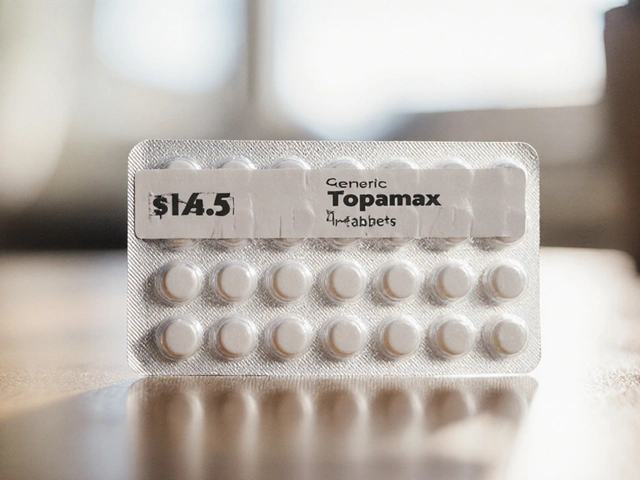
Buy Cheap Generic Topamax Online - Safe Guide & Price Comparison
By Marcel Kornblum Oct 9, 2025

Why Real Customers Are Leaving CanadaDrugsDirect: Honest Stories & Alternatives
By Marcel Kornblum Apr 24, 2025

