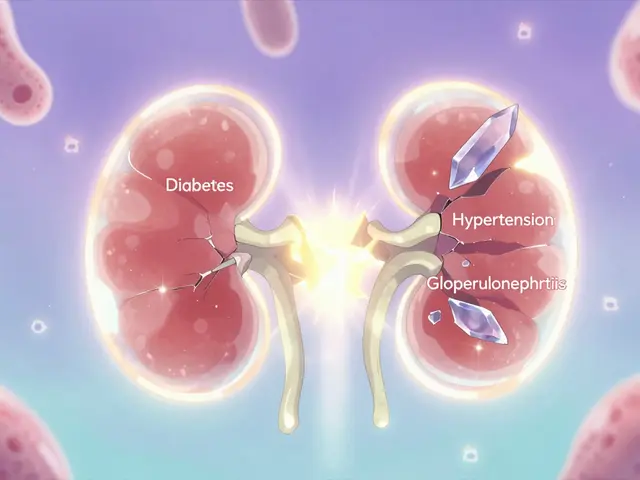
When your insurance company says generic medication is good enough-but it’s making you sicker or just not working-you’re not alone. Thousands of people face this every year. You’ve been told the generic is "bioequivalent," but your body says otherwise. Your seizures are back. Your thyroid levels are out of control. Your depression won’t lift. The pill that worked for years suddenly doesn’t. And now your insurer won’t cover the brand-name version anymore. That’s not just frustrating. It’s dangerous.
Why Generics Don’t Always Work the Same
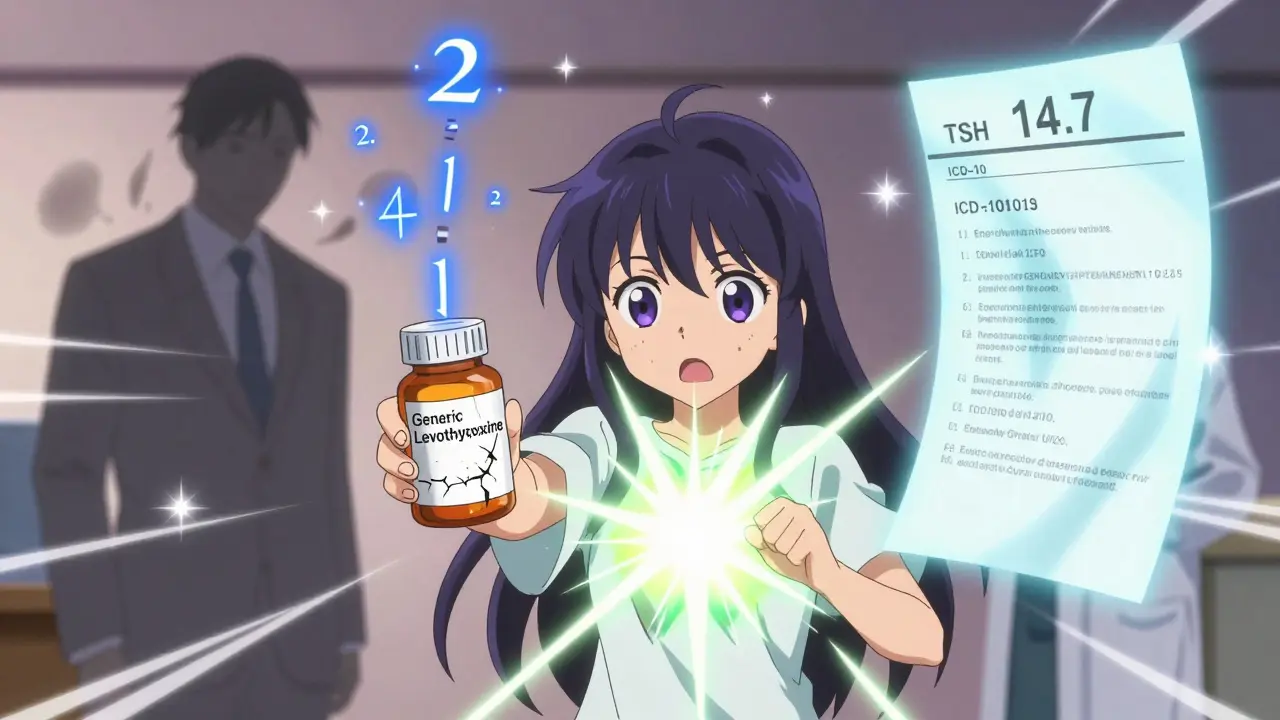
The FDA says generics must deliver 80% to 125% of the active ingredient compared to the brand-name drug. Sounds fair, right? But for some medications, that 45% window is huge. Think of it like this: if you need exactly 50 milligrams of a drug to stay stable, a generic could give you anywhere from 40 to 62.5 milligrams. For drugs like levothyroxine, warfarin, or antiepileptics, even small changes in blood levels can cause serious problems. Patients with epilepsy have reported breakthrough seizures after switching to a generic levetiracetam. People on thyroid meds have seen TSH levels jump from 2.1 to 14.7 after switching to a generic levothyroxine. These aren’t rare cases. Studies show 15% to 20% of patients experience therapeutic failure with certain generics, especially for narrow-therapeutic-index drugs.What Insurance Says vs. What You Know
Your insurer’s denial letter probably says something like: "A generic alternative is available and preferred under your plan." They don’t care that you’ve tried three different generics. They don’t care that your doctor wrote a letter. They don’t care that you’ve been hospitalized twice since the switch. Their job is to cut costs. And generics are cheaper-90% of prescriptions are generic, but they only make up 23% of total drug spending. So when you ask for the brand name, they say no. Unless you fight back.The Appeal Process: Step by Step
You have rights. The Affordable Care Act and state laws give you a clear path to appeal. Here’s how it works:- Get your Explanation of Benefits (EOB)-this is your denial letter. Look for codes like DA2000 (generic available) or DA1200 (not on formulary). Keep it. You’ll need it.
- Call your doctor. Don’t just ask them to write a letter. Schedule a 30-minute appointment specifically for this. Bring your symptom log: dates you switched, what you felt, lab results, hospital visits. The more detail, the better.
- Get a detailed physician letter. Generic appeals fail because doctors write vague things like "Patient needs brand name." Successful appeals say: "Patient experienced TSH increase from 2.1 to 14.7 mIU/L within 8 weeks of switching from Synthroid to generic levothyroxine. Reversion to Synthroid normalized TSH to 2.4 within 6 weeks. This meets Endocrine Society guidelines for therapeutic inequivalence." Include ICD-10 codes. Reference FDA labeling. Cite clinical guidelines.
- Submit your internal appeal. You have 180 days for commercial plans, 60 days for Medicare Part D. Use certified mail. Keep copies of everything.
- If denied again, request an external review. This is where most wins happen. An independent third party reviews your case. Studies show 67% of external appeals are approved when documentation is solid.
- For Medicare patients, there are more steps: Office of Medicare Hearings and Appeals, then the Medicare Appeals Council. Deadlines matter. Don’t miss them.
What Makes an Appeal Succeed
It’s not luck. It’s evidence. The Patient Advocate Foundation analyzed over 12,000 appeals. The difference between approval and denial? Documentation.- Lab results showing subtherapeutic levels (e.g., TSH, INR, drug blood levels)
- Medication logs tracking symptoms before and after switch
- Physician letter with specific clinical reasoning, not just opinion
- Proof of failed attempts with other generics or biosimilars
- References to official guidelines (Endocrine Society, Epilepsy Foundation, etc.)

Where the System Fails
Some insurers demand you try three or even six generics before even considering the brand name. That’s called step therapy. But 28 states now ban this for documented therapeutic failures. If you’re in one of those states, say so in your appeal. If you’re not, still push back-especially if you’ve had hospitalizations or seizures. Another problem? Insurers claim there’s "no clinical evidence" of failure-even when you’ve got blood tests, ER records, and doctor notes. That’s not just wrong. It’s deceptive. Dr. David Nash, former FDA advisor, calls it "creating artificial barriers to medically necessary care." And it’s happening more often.Tools and Help That Actually Work
You don’t have to do this alone.- GoodRx Appeal Assistant-free tool that generates a custom appeal letter based on your medication and insurance. Users report 4.7/5 stars. Doctors say it makes signing the letter 10 times faster.
- Patient Advocate Foundation (1-800-532-5274)-free case management. They help you organize records, write letters, and track deadlines. 92% satisfaction rate in 2023.
- Specialty pharmacies like OptumRx and Accredo offer appeal support. Their clients have a 73% approval rate versus 51% for self-managed appeals.
- Non-profits like the Crohn’s & Colitis Foundation and Epilepsy Foundation have downloadable appeal kits with templates, checklists, and sample letters.
Success Rates by Condition and Plan Type
Not all appeals are created equal. Your odds depend on what you’re treating and what kind of insurance you have.| Condition | Success Rate | Insurance Type |
|---|---|---|
| Thyroid (levothyroxine) | 89% | Medicare Part D |
| Seizure disorders (levetiracetam) | 78% | Commercial |
| Antidepressants | 45% | Commercial |
| Warfarin | 72% | Medicare |
| All types (average) | 67% | External review |
| All types (average) | 39% | Initial commercial appeal |
What’s Changing in 2025
The system is slowly improving. In 2024, CMS mandated that insurers process appeals for anti-seizure drugs within 72 hours. That’s huge. The FDA is also drafting new guidance on "individualized bioequivalence," which could mean future generics are tested for patient-specific responses. Meanwhile, 19 states now have "right to try brand" laws: if you’ve had two documented failures with generics, your insurer must cover the brand name. But the biggest change? More doctors are finally learning how to write effective appeal letters. The American Medical Association released new templates in 2024-standardized, insurer-friendly, and packed with the right terms. If your doctor hasn’t updated their approach, ask them to.Don’t Give Up
You’ve been told to accept the generic. But your body isn’t a spreadsheet. It’s not a cost center. It’s you. And you deserve a medication that works. The system is stacked against you-but it’s not unbeatable. 68% of people get denied at first. But 52% win after appealing. That’s more than half. You’re not asking for luxury. You’re asking for basic medical care. And you have the right to fight for it.What if my doctor won’t help me with the appeal?
If your doctor refuses, contact the Patient Advocate Foundation (1-800-532-5274). They can help you draft a letter and even reach out to your provider on your behalf. Many doctors are willing to help once they understand how critical it is-especially if you show them lab results or hospital records. You can also ask for a referral to a pharmacist who specializes in medication therapy management-they often have experience with insurance appeals.
How long does an insurance appeal take?
Internal appeals take 14 to 30 days for commercial plans, 7 days for Medicare. External reviews take 30 to 45 days. If your condition is urgent-like seizures, unstable thyroid levels, or bleeding risk from warfarin-you can request an expedited review. Medicare must respond within 72 hours for urgent cases. Make sure your doctor marks the appeal as "urgent" and explains why delay could cause harm.
Can I get the brand-name drug while waiting for approval?
Sometimes. Some insurers offer temporary coverage through an emergency exception while your appeal is pending. Ask your pharmacist or case manager. If you’re on Medicare, you may qualify for a 30-day emergency supply if your medication was previously covered. If you’re running out, contact the Patient Advocate Foundation-they’ve helped people get bridge prescriptions from drug manufacturers.
Are there any new laws that help with these appeals?
Yes. In 2023, 19 states passed "right to try brand" laws requiring insurers to cover brand-name drugs after two documented generic failures. The 2024 Consolidated Appropriations Act also requires insurers to use real-time benefit tools so doctors know coverage status before prescribing. And Medicare now eliminates cost-sharing for approved appeals-meaning if you win, you don’t pay extra for the brand-name drug.
What if my appeal is still denied after external review?
For commercial insurance, you can file a complaint with your state’s insurance commissioner. For Medicare, you can appeal to the Medicare Appeals Council and, if needed, take it to federal court. Most people stop here-but you’re not out of options. Organizations like the Patient Advocate Foundation and National Health Law Program can help you navigate the next steps. In some cases, media exposure or public pressure has forced insurers to reverse decisions.
Next Steps: What to Do Today
If you’re facing a denial:- Grab your EOB and check the denial code.
- Start a symptom log if you haven’t already-date, dosage, side effects, lab values.
- Call your doctor and ask for a dedicated appointment to write the appeal letter.
- Visit GoodRx’s Appeal Assistant tool and generate a draft.
- Submit your appeal within 14 days-don’t wait.




ANA MARIE VALENZUELA
December 28, 2025 at 08:03
This is why generic drug companies should be sued for fraud. 80%-125%? That’s not bioequivalent-that’s a roulette wheel with your life. I had a cousin who had three seizures in two weeks after switching to generic Keppra. The ER doctor said, 'You’re lucky you didn’t die.' And the insurance rep just said, 'The generic is FDA-approved.' Yeah, and so is a chainsaw if you use it right. Stop pretending this is science. It’s corporate greed in a white coat.