Antidepressants for Seniors: Safe Options, Side Effects, and What Works Best
When treating antidepressants for seniors, medications used to treat depression in older adults, often with different risks and benefits than in younger patients. Also known as geriatric antidepressants, these drugs must be chosen carefully because aging changes how the body absorbs, processes, and responds to medication. Depression isn’t a normal part of getting older—but it’s common. About 7% of adults over 65 struggle with it, and many go untreated because symptoms look like fatigue, memory loss, or just "being grumpy." The right antidepressant can bring back energy, sleep, and joy—but the wrong one can cause falls, confusion, or dangerous drug interactions.
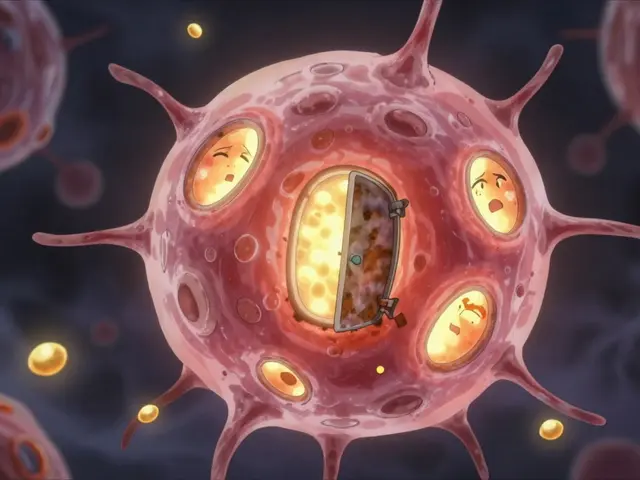
SSRIs, a class of antidepressants that increase serotonin levels in the brain, commonly prescribed for older adults due to their safety profile. Also known as selective serotonin reuptake inhibitors, they include drugs like sertraline and escitalopram, which are often first choices for seniors because they’re less likely to cause dizziness or dry mouth than older types. But even SSRIs aren’t risk-free. In older adults, they can lower sodium levels, leading to confusion or weakness—a condition called hyponatremia. That’s why doctors start low and go slow. Another key player is venlafaxine, an SNRI antidepressant that affects both serotonin and norepinephrine, sometimes used when SSRIs don’t work. Also known as Effexor, it can help with pain and fatigue too, but it may raise blood pressure, so it’s not ideal for people with heart issues. Then there’s mirtazapine, an antidepressant that improves sleep and appetite, often chosen for seniors who’ve lost weight or can’t sleep. Also known as Remeron, it’s not a first-line choice for everyone, but for someone who’s withdrawn and eating poorly, it can be a game-changer.
What makes antidepressants for seniors tricky isn’t just the drug itself—it’s what else they’re taking. Many older adults are on blood pressure pills, heart meds, or painkillers. Mixing antidepressants with these can lead to serious problems. For example, combining an SSRI with a blood thinner like warfarin increases bleeding risk. Or using an SSRI with certain pain meds can trigger serotonin syndrome—a rare but dangerous spike in brain serotonin. That’s why pharmacogenetic testing is gaining traction: some people metabolize these drugs too slowly or too fast because of their genes. Studies show this testing cuts adverse reactions by 30%, making treatment safer. And it’s not just about pills. Depression in seniors often ties to loneliness, chronic pain, or mobility loss. Antidepressants help, but they work best when paired with therapy, movement, or social engagement.
You’ll find real stories below—not theory, but what actually works in clinics and homes. Some seniors respond better to low-dose sertraline. Others need to avoid certain meds entirely because of kidney function or heart rhythm concerns. We cover what to watch for, which drugs are safest long-term, and how to tell if the treatment is helping—or hurting. No fluff. Just clear, practical info for families and older adults navigating this complex space.
Older Adults on SSRIs: How to Prevent Hyponatremia and Falls
SSRIs help treat depression in older adults but raise the risk of hyponatremia and falls. Learn how to spot early signs, which antidepressants are safest, and what tests you should ask for to stay safe.
About
Medications
Latest Posts


Atomoxetine and Anxiety: Can it Help or Hurt?
By Marcel Kornblum May 5, 2023

Fulvicin (Griseofulvin) vs. Top Antifungal Alternatives: What Works Best Today
By Marcel Kornblum Oct 30, 2025
Type 2 Diabetes: How Insulin Resistance Leads to Metabolic Syndrome
By Marcel Kornblum Mar 4, 2026

