PPI Therapy: What It Is, How It Works, and What You Need to Know
When you’re dealing with constant heartburn or a sour taste in your mouth, PPI therapy, a treatment using proton pump inhibitors to reduce stomach acid production. Also known as proton pump inhibitor therapy, it’s one of the most common ways doctors manage acid-related conditions like GERD and peptic ulcers. But PPIs aren’t just quick fixes—they change how your stomach works, and that comes with real trade-offs.
Proton pump inhibitors like omeprazole, esomeprazole, and pantoprazole block the final step of acid production in stomach cells. That means less acid, less burning, and fewer ulcers. But here’s what most people don’t realize: your body needs some stomach acid to digest food, kill bacteria, and absorb nutrients like magnesium, calcium, and vitamin B12. Long-term use can lead to deficiencies, bone fractures, or even gut infections like C. diff. Studies show that people on PPIs for over a year have a 25% higher risk of hip fractures compared to those who don’t use them.
That’s why PPI therapy isn’t one-size-fits-all. For some, it’s life-changing—someone with Barrett’s esophagus or a history of bleeding ulcers might need it for years. But for others, especially those with mild heartburn, lifestyle changes or H2 blockers like famotidine work just as well—with fewer side effects. And if you’ve been on PPIs for more than a few months without a clear reason, it’s worth asking your doctor if you can taper off. Many people find their symptoms improve once they adjust their diet, lose weight, or stop eating late at night.
Related to PPI therapy are other tools that affect stomach acid: H2 blockers, medications that reduce acid by blocking histamine receptors. Also known as histamine-2 receptor antagonists, they’re often used for short-term relief and are less likely to cause long-term nutrient issues. Then there’s antacids, fast-acting, over-the-counter options like Tums or Maalox that neutralize acid on contact. Also known as acid neutralizers, they’re great for occasional heartburn but don’t stop acid production like PPIs do. And let’s not forget lifestyle factors—alcohol, caffeine, spicy food, and lying down after meals can all make acid reflux worse, no matter how much medication you take.
What you’ll find in the articles below isn’t just a list of PPIs. It’s a collection of real, practical insights—like how generic substitution can affect seizure control in people taking antiseizure drugs, or how inactive ingredients in pills might trigger reactions in sensitive people. You’ll see how drug pricing affects access, how supplements like evening primrose oil can interfere with brain chemistry, and how something as simple as massage therapy can help with digestive issues tied to stress. These aren’t random posts. They’re all connected by one truth: medications don’t work in a vacuum. Your body, your diet, your genetics, and your environment all play a role. And understanding that is the first step to using PPI therapy—or any drug—safely and effectively.
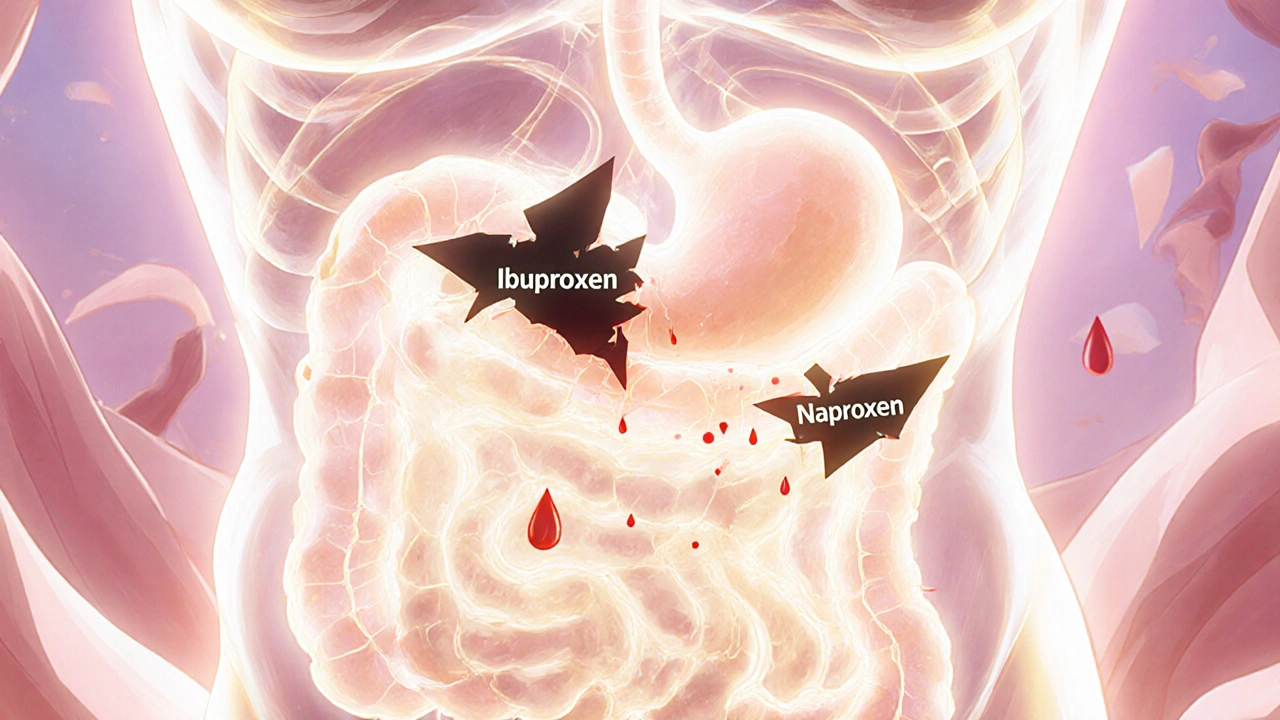
NSAIDs and Peptic Ulcer Disease: Understanding the Risk of Gastrointestinal Bleeding
NSAIDs like ibuprofen and naproxen can cause serious gastrointestinal bleeding, especially in older adults or those with risk factors. Learn how to recognize the signs, reduce your risk, and use safer alternatives.
About
Medications
Latest Posts


How to Buy Cheap Generic Metformin Online - A Safe, Fast Guide
By Marcel Kornblum Sep 24, 2025

Hidden Signs of Vitamin Deficiency in Nails, Skin, and Hair
By Marcel Kornblum Oct 10, 2025

Authorized Generics: How Brand Drug Companies Respond to Patent Expiration
By Marcel Kornblum Dec 1, 2025