Refrigerate Medications: What You Need to Know About Storage and Safety
When you refrigerate medications, store certain drugs at controlled cold temperatures to preserve their potency and safety. Also known as cold-chain storage, this practice isn’t optional for some drugs—it’s critical to their function. If you leave insulin, certain antibiotics, or eye drops out of the fridge when they need it, you could be taking a drug that no longer works—or worse, one that’s degraded into something harmful.
Not every medicine needs the fridge, but the ones that do are often life-changing or life-saving. Insulin, a hormone used to manage diabetes, is one of the most common temperature-sensitive drugs. Once opened, many insulin pens and vials last 28 days at room temperature—but unopened ones must stay cold. If you don’t refrigerate them before first use, they can lose potency before you even take your first dose. Eye drops, especially those for glaucoma or infections, often require refrigeration after opening to prevent bacterial growth and maintain chemical stability. Liquid antibiotics like amoxicillin suspension also degrade quickly at room temperature, sometimes becoming ineffective within days.
It’s not just about the fridge, though. Where you put it matters too. Storing meds in the door of the refrigerator exposes them to constant temperature swings every time you open it. The back shelf, where it’s coldest and most stable, is better. And never freeze anything unless the label says to—freezing can break down the structure of some liquids and injectables. Light exposure is another silent killer: if your medication comes in a clear bottle and says to protect from light, wrap it in aluminum foil or store it in its original box. You wouldn’t leave coffee beans in the sun, so don’t do the same to your meds.
Some people think generics are more forgiving with storage, but that’s a myth. Whether it’s brand or generic, if the active ingredient is the same, the storage rules are too. A study from the FDA found that improperly stored antiseizure drugs, like carbamazepine, showed measurable drops in concentration after just a few days at room temperature when they were supposed to be refrigerated. That’s not a small risk—it’s a seizure waiting to happen.
Traveling with refrigerated meds? Use a small insulated cooler with ice packs, not just a ziplock bag. Airlines let you carry them in your hand luggage, even if they’re liquids. Just bring a doctor’s note or the original prescription label. Pharmacies can also help—some offer cold shipping for mail-order meds. And always check the label. If it says "refrigerate" or "store between 36°F and 46°F," don’t guess. That’s not a suggestion—it’s a requirement.
Expired meds are dangerous, but so are meds that were never stored right. You can’t tell by looking if a drug has broken down. One pill might look fine, but if it’s insulin that got too warm, your blood sugar could spike without warning. That’s why creating a simple medication expiration review schedule isn’t just smart—it’s protective. Check your fridge meds monthly. Write the date you opened them on the bottle. If you’re unsure, call your pharmacist. They’ve seen what happens when people assume their meds are fine.
Below, you’ll find real-world advice on how to store everything from insulin to eye drops, what to do when power goes out, and how to tell if your meds have gone bad. These aren’t theory pages—they’re guides written by people who’ve been there, who’ve had to fix mistakes, and who know what actually works when your health depends on it.
How to Manage Medication Storage in Shared Living Spaces: Safety, Security, and Smart Systems
Learn how to safely store medications in shared homes with tips on locking, refrigerating, labeling, and disposing of pills. Avoid accidents, misuse, and expired drugs with practical steps for families and caregivers.
About
Medications
Latest Posts

Cleocin (Clindamycin) vs. Alternatives: A Practical Comparison
By Marcel Kornblum Sep 29, 2025

Inactive Ingredient Differences: Can Excipients Affect Safety or Efficacy?
By Marcel Kornblum Nov 12, 2025
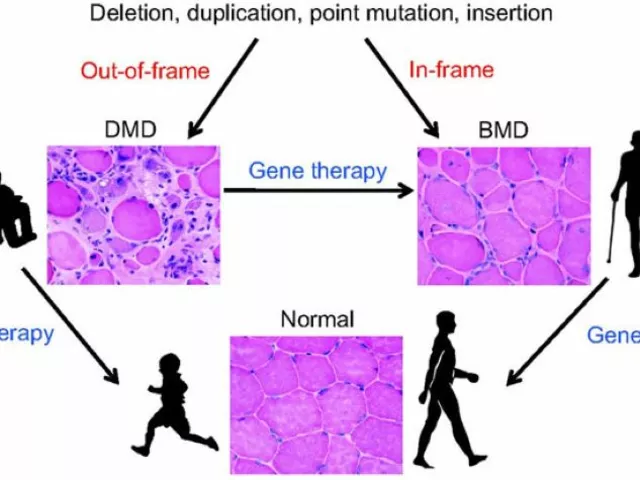
Coping with a Duchenne Muscular Dystrophy Diagnosis: Tips for Parents
By Marcel Kornblum Jul 26, 2023