Drug Shortages: What Causes Them and How They Impact Your Medications
When your pharmacy says they’re out of your usual pill, it’s not just bad luck—it’s a drug shortage, a period when the supply of a medication falls below demand, making it hard or impossible to get the drug you need. Also known as medication supply crisis, these gaps don’t just delay treatment—they can force dangerous switches, increase costs, and even put lives at risk. This isn’t rare. In 2023 alone, over 300 drugs faced shortages in the U.S., including common ones like insulin, antibiotics, and blood pressure meds. It’s not about one factory failing—it’s a broken system.
Behind every drug shortage, a period when the supply of a medication falls below demand, making it hard or impossible to get the drug you need. Also known as medication supply crisis, these gaps don’t just delay treatment—they can force dangerous switches, increase costs, and even put lives at risk. is a tangled web of causes. One big factor is generic drug manufacturing, the production of off-patent medications that make up over 90% of prescriptions but rely on a tiny number of overseas factories with shaky quality control.low-cost generic production. When one plant in India or China gets shut down by the FDA for unsanitary conditions, it can knock out half the country’s supply of a common drug. Then there’s pharmacy supply chain, the network of distributors, wholesalers, and Pharmacy Benefit Managers (PBMs) that control how drugs move from makers to your hands.pharmaceutical distribution network. PBMs often push for the cheapest version, even if it’s harder to produce or less reliable. That means manufacturers skip production if the profit is too thin. And when a drug is only made by one or two companies? One hiccup = nationwide shortage.
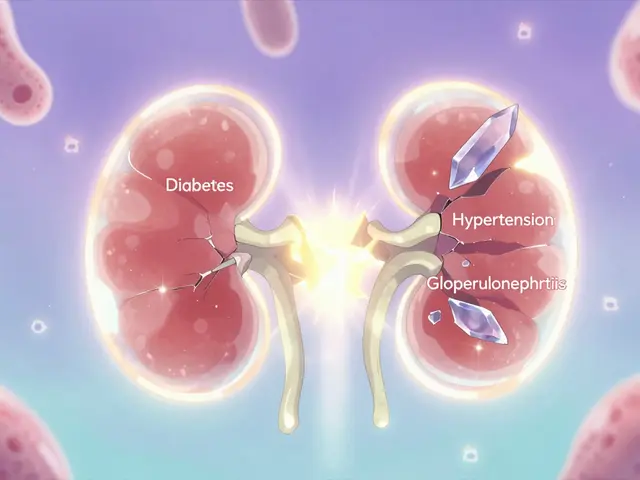
These shortages hit hardest for people on chronic meds—like those taking antiseizure drugs, immunosuppressants, or blood thinners. Switching brands or generics isn’t safe for everyone. A tiny change in how a drug is absorbed can trigger a seizure, rejection of a transplant, or a dangerous blood clot. Even inactive ingredients, the non-active components in pills like fillers, dyes, and binders that can affect how a drug works or trigger reactions in sensitive people.excipients matter. One manufacturer’s version might use a different binder that causes stomach upset or slows absorption. You might not know until you’re stuck with a substitute that doesn’t work like your usual pill.
And it’s not just about getting your meds. Shortages force doctors to pick less effective alternatives, delay treatments, or push patients toward pricier brand-name drugs—sometimes without insurance coverage. The system is designed to cut costs, but the real cost is your health. The good news? You’re not powerless. Knowing which drugs are most at risk, asking your pharmacist about alternatives, and understanding how your insurance handles substitutions can help you stay ahead. Below, you’ll find real stories and practical guides from people who’ve been through this—how to spot the signs of a shortage, what to say to your doctor, and how to find safe, affordable options when your usual pill isn’t there.
Natural Disasters and Drug Shortages: How Climate Change Is Cutting Off Life-Saving Medicines
Natural disasters like hurricanes are causing life-threatening drug shortages by damaging key pharmaceutical manufacturing sites. With 65% of U.S. drug facilities in disaster-prone areas, the system is fragile-and patients are paying the price.
Congressional Bills to Tackle Drug Shortages: What’s Really in the Works
Two congressional bills aim to fix worsening drug shortages, but both are stuck in limbo due to the longest government shutdown in U.S. history. Here's what they do - and why they might never pass.
About
Medications
Latest Posts


Alternate-Day Statin Dosing: Can It Lower LDL Without Side Effects?
By Marcel Kornblum Jan 20, 2026

Why You Shouldn’t Store Medications in the Bathroom
By Marcel Kornblum Jan 17, 2026

Hidden Signs of Vitamin Deficiency in Nails, Skin, and Hair
By Marcel Kornblum Oct 10, 2025